Introduction
Renal dysfunction is a recognized risk factor for mortality after HCT, as it is included in the comorbidity index (HCT CI). Yet, further understanding on outcomes in patients with different level of renal dysfunction or undergoing hemodialysis (HD) at time of transplant remains scant. This study explores the impact of different levels renal dysfunction on major HCT outcomes in a large population using data reported to the Center for International Blood and Marrow Transplant Research (CIBMTR).
Methods
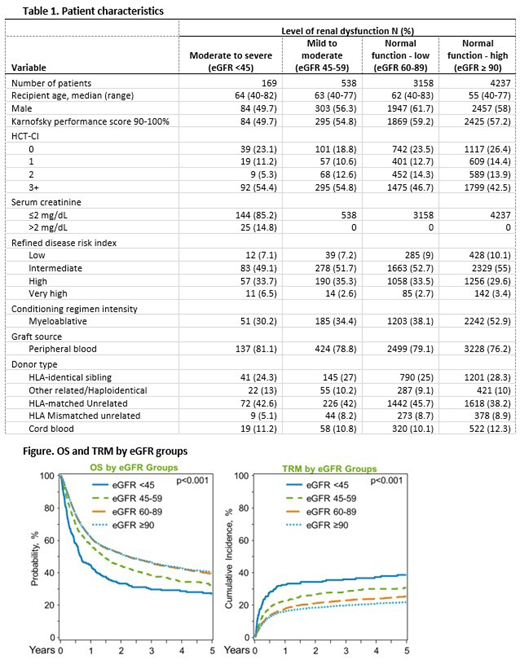
The study population included 8,102 patients age 40 years and older who received HCT for treatment of malignancies from 2008 to 2016, with available pre-transplant creatinine measurement. eGFR, calculated using CKD-EPI (CKD-epidemiology collaboration) method, was used to assigned patients in four categories: eGFR ≥ 90ml/min (eGFR≥ 90, N=4,237, reference), eGFR 60-90ml/min (eGFR 60-90, N=3,158), eGFR 45-59ml/min (eGFR 45-59, N=538) and eGFR <45ml/min(eGFR<45, N=169). A separate cohort of patients on HD at time of HCT (N=46) was analyzed independently. Multivariate analysis models were built for assessment of overall mortality, transplant-related mortality (TRM), disease relapse or progression, graft-versus-host disease (GVHD), hepatic sinusoidal obstructive syndrome (SOS), thrombotic microangiopathy (TMA), idiopathic pneumonia syndrome (IPS) and need of HD post-transplant. Common patient-, disease- and transplant-related covariates were tested on all models and HCT CI was computed without reported renal dysfunction comorbidity to avoid collinearity.
Results
Patient characteristics are shown in table 1. The groups were comparable on disease risk index, graft and donor source, but patients with eGFR>90 were younger and received myeloablative conditioning more frequently. The cohort of eGFR <45 had a higher proportion of patients with HCT CI ≥3. TRM and overall survival according to eGFR groups are shown in Figure. In the multivariate analysis models eGFR as the main effect was associated with TRM (p<0.0001), overall mortality (p<0.0001), and requirement of HD post HCT (p<0.0001), but not for relapse/progression (p=0.98), GVHD (grades II-IV, p=0.34; III-IV, p=0.70; and chronic, p=0.20), TMA (p=0.46), SOS (p=0.02) or IPS (p=0.06). Compared to eGFR ≥90, the hazard ratio (HR) for TRM for eGFR 60-89 was 1.12 (p=0.07), for eGFR 45-59 was 1.46 (p<0.001) and for eGFR<45 was 1.74 (p=0.004). Corresponding HRs for overall mortality were 1.0 (p=0.9), 1.17 (p=0.03) and 1.63 (p<0.0001), respectively. Similarly, for the need of HD post HCT, HR for eGFR60-89 was 1.29 (p=0.03), eGFR45-59 was 2.45 (p<0.001) and for eGFR<45 was 3.09 (p<0.0001). Only eGFR<45 was associated with higher risk of SOS (HR2.66, p=0.03). Among 46 patients on HD prior to HCT, one-year probability of overall survival was 20% (95% Confidence Interval [CI] 10-32%) and cumulative incidence of TRM at one year was 67% (95% CI, 50-81%).
Conclusion
These findings indicate that degree of renal dysfunction is an independent predictor of OS, TRM, probability of receiving HD and SOS when adjusted for other risk factors. The impact of eGFR on the need of HD, a complication that increases morbidity post HCT is an important finding. Additionally, the outcomes of a subset of patients on HD at time of transplants are dismal. These results can further assist the prognostic assessment of candidates for an allogeneic HCT.
Stadtmauer:Celgene: Consultancy; Takeda: Consultancy; Janssen: Consultancy; Amgen: Consultancy; Novartis: Consultancy, Research Funding; Tmunity: Research Funding; Abbvie: Research Funding. Wingard:Ansun: Consultancy; Pluristem: Consultancy; Celgene: Consultancy; Merck: Consultancy; Shire: Consultancy. Ganguly:Seattle Genetics: Speakers Bureau; Daiichi Sankyo: Research Funding; Kite Pharma: Honoraria, Other: Advisory Board; Janssen: Honoraria, Other: Advisory Board. Pasquini:Pfizer: Other: Advisory Board; Amgen: Consultancy; Medigene: Consultancy; BMS: Research Funding; Novartis: Research Funding; Kit Pharma: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal