Introduction: Daratumumab (DARA), a human, IgGκ monoclonal antibody targeting CD38, is approved either as a single agent or in combination with anti-myeloma regimens for newly diagnosed MM (NDMM) or relapsed/refractory MM (RRMM). In phase 3 studies, DARA-based regimens reduced the disease progression or death risk by ≥44%, nearly doubled the rates of complete response (CR) or better, and tripled minimal residual disease (MRD)-negativity rates (10-5 sensitivity threshold) in NDMM or RRMM pts (Palumbo A, et al. N Engl J Med 2016. 375[8]:754-766; Dimopoulos MA, et al. N Engl J Med 2016. 375[14]:1319-1331; Mateos MV, et al. N Engl J Med 2018. 378[6]:518-528; Facon T, et al. N Engl J Med 2019. 380[22]2104-2015). In the phase 3 CASTOR study (median follow-up 40.0 mo), D-Vd reduced the risk of disease progression or death by 69% and induced higher rates of deeper responses vs Vd in RRMM pts. Pts who received 1 prior line (PL) of therapy achieved the greatest benefit with D-Vd. Here, we examine updated (47.0 mo median follow-up) efficacy and safety of D-Vd vs Vd in CASTOR, with a focus on pts with 1 PL of therapy.
Methods: In CASTOR, pts were randomized to 8 cycles (21 d/cycle) of V (1.3 mg/m2, SC) on Days 1, 4, 8, and 11 and dexamethasone (20 mg, PO or IV) on Days 1, 2, 4, 5, 8, 9, 11, and 12 ± DARA (16 mg/kg, IV) given weekly for Cycles 1-3, Q3W for Cycles 4-8, and Q4W thereafter. Cytogenetic risk was evaluated by local fluorescence in situ hybridization or karyotyping; high risk was defined as the presence of t(4;14), t(14;16), or del17p abnormalities.
Results: A total of 498 pts were randomized (D-Vd, n = 251; Vd, n = 247) and included in the intent-to-treat (ITT) population. A total of 235 pts had 1 PL of therapy (D-Vd, n = 122; Vd, n = 113).
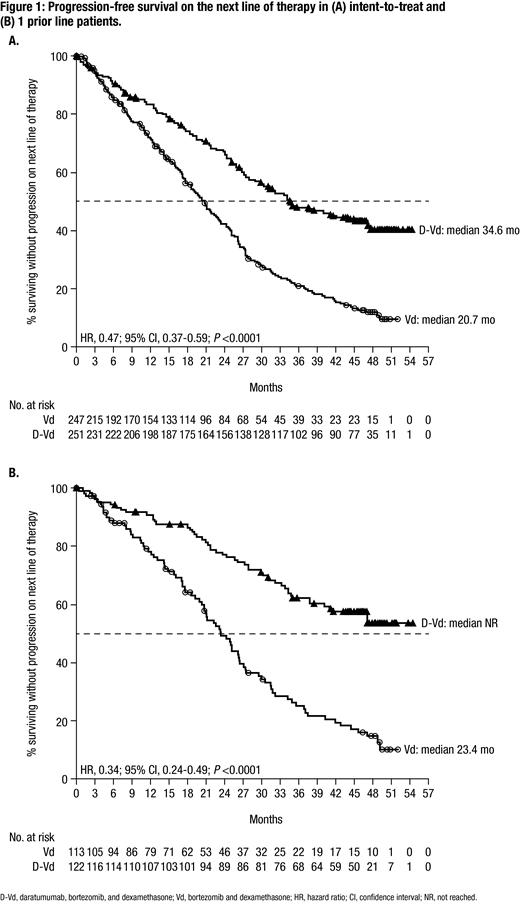
After a median follow-up of 47.0 mo, progression-free survival (PFS) was significantly prolonged with D-Vd vs Vd in the ITT population (median: 16.7 vs 7.1 mo; HR, 0.31; 95% CI, 0.25-0.39, P <0.0001). The PFS benefit for D-Vd vs Vd was maintained in pts with prior V (median: 12.1 vs 6.7 mo; HR, 0.34; 95% CI, 0.26-0.46, P <0.0001), with prior R (median: 9.5 vs 6.1 mo; HR, 0.40; 95% CI, 0.28-0.58, P <0.0001), and high (median: 12.6 vs 6.2 mo; HR, 0.41; 95% CI, 0.21-0.83, P = 0.0106) and standard cytogenetic risk (median: 16.6 vs 6.6 mo; HR, 0.26; 95% CI, 0.18-0.36, P <0.0001). D-Vd significantly prolonged PFS on the subsequent line of therapy (PFS2) vs Vd (median: 34.6 vs 20.7 mo; HR, 0.47, 95% CI, 0.37-0.59; P <0.0001; Figure 1A). At the time of analysis, 114 deaths with D-Vd and 132 deaths with Vd were observed with 3-yr overall survival (OS) rates of 61% vs 51%, respectively; follow-up for OS is ongoing. The overall response rate (ORR; 85% vs 63%), ≥very good partial response (VGPR) rate (63% vs 29%) and ≥CR rate (30% vs 10%) were all significantly higher (all P <0.0001) with D-Vd vs Vd.
Among 1 PL pts, median PFS was 27.0 vs 7.9 mo (HR, 0.21; 95% CI, 0.15-0.31, P <0.0001) for D-Vd vs Vd. The PFS benefit for D-Vd vs Vd was maintained among 1 PL pts previously exposed to V (median: 20.4 vs 8.0 mo; HR, 0.22; 95% CI, 0.13-0.37; P <0.0001) or R (median: 21.2 vs 7.0 mo; HR, 0.30; 95% CI, 0.11-0.82; P = 0.0140). PFS2 was also significantly prolonged with D-Vd vs Vd in 1 PL pts (median: not reached vs 23.4 mo; HR, 0.34, 95% CI, 0.24-0.49; P <0.0001; Figure 1B); 42-mo PFS2 rates were 58% vs 19%, respectively. For 1 PL pts, 39 vs 56 deaths were observed with D-Vd vs Vd, with 3-yr OS rates of 76% vs 57%, respectively. ORR (92% vs 74%; P = 0.0007) and rates of ≥VGPR (77% vs 42%; P <0.0001) and ≥CR (43% vs 15%; P <0.0001) were all significantly higher with D-Vd vs Vd.
Additional data including MRD analyses will be presented.
The most common (≥5%) grade 3/4 treatment-emergent adverse events (TEAEs) with D-Vd vs Vd included thrombocytopenia (46% vs 33%), anemia (16% vs 16%), neutropenia (14% vs 5%), pneumonia (10% vs 10%), lymphopenia (10% vs 3%), hypertension (7% vs 1%), and peripheral sensory neuropathy (5% vs 7%). Discontinuation rates due to TEAEs were similar for D-Vd vs Vd (10% vs 9%). The rate of invasive second primary malignancy rates were 4.9% in the D-Vd group vs 1.7% in the Vd group.
Conclusions: In this updated analysis of CASTOR, D-Vd maintains significant PFS and ORR benefits in RRMM, with the greatest benefit achieved by pts who received 1 PL of therapy. The safety profile of D-Vd remains consistent with longer follow-up, with no new safety concerns reported. These data continue to suggest that administration of D-Vd to RRMM pts after first relapse may provide the greatest clinical benefit.
Weisel:Juno: Consultancy; Adaptive Biotech: Consultancy, Honoraria; GSK: Honoraria; Takeda: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Celgene Corporation: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Research Funding. Sonneveld:SkylineDx: Research Funding; Takeda: Honoraria, Research Funding; Karyopharm: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; BMS: Honoraria. Mateos:Adaptive: Honoraria; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; EDO: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees; Pharmamar: Membership on an entity's Board of Directors or advisory committees. Hungria:BMS: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Consultancy, Honoraria, Speakers Bureau; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Spencer:Sanofi: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Haemalogix: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Secura Bio: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Specialised Therapeutics Australia: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen Oncology: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Servier: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Estell:Janssen/ Celgene: Membership on an entity's Board of Directors or advisory committees. Barreto:Hemocentro, USP-Ribeira; Preto-SP: Employment. Corradini:Gilead: Honoraria, Other: Travel Costs; AbbVie: Consultancy, Honoraria, Other: Travel Costs; Amgen: Honoraria; Celgene: Honoraria, Other: Travel Costs; Daiichi Sankyo: Honoraria; BMS: Other: Travel Costs; Takeda: Honoraria, Other: Travel Costs; Servier: Honoraria; Kite: Honoraria; Novartis: Honoraria, Other: Travel Costs; Roche: Honoraria; Sanofi: Honoraria; KiowaKirin: Honoraria; Janssen: Honoraria, Other: Travel Costs; Jazz Pharmaceutics: Honoraria. Krevvata:Janssen: Employment. Trivedi:Janssen: Employment, Equity Ownership. Qin:Janssen: Employment, Equity Ownership. Pei:Janssen: Employment, Equity Ownership. Ukropec:Janssen: Employment, Equity Ownership. Kobos:Janssen: Employment. Qi:Janssen: Employment. Nooka:Amgen: Honoraria, Other: advisory board participation; BMS: Honoraria, Other: advisory board participation; Adaptive technologies: Honoraria, Other: advisory board participation; Janssen: Honoraria, Other: advisory board participation; Celgene: Honoraria, Other: advisory board participation; Takeda: Honoraria, Other: advisory board participation; GSK: Honoraria, Other: advisory board participation; Spectrum pharmaceuticals: Honoraria, Other: advisory board participation.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal