Introduction: Patients (pts) with high-risk multiple myeloma (HRMM) experience early disease progression post autologous stem cell transplant (ASCT). The median progression free survival (PFS) for HRMM pts undergoing ASCT with lenalidomide (len) maintenance ranges between 27 and 42 months in high risk pts and 22 months in ultra-high risk, defined by two or more adverse cytogenetic abnormalities such as: gain(1q), t(4;14), t(14;16),t(14;20), or del(17p)( Chakraborty et al, Leukemia,2018 and Jackson et al, Lancet, 2018). Elotuzumab, a humanized IgG kappa monoclonal antibody against SLAM-F7 (CS-1), is approved in combination with len and dexamethasone (ERd) in pts with relapsed MM (Dimopoulus et al, BJH, 2017). It directly activates natural killer (NK) cells and mediates myeloma cell death by antibody-dependent cell mediated cytoxicity. We hypothesized that administration of ERd as post-ASCT consolidation will enhance an immune-competent phenotype, by restoring NK cells and effector T-cell populations at a time of maximal disease de-bulking, and will ultimately improve outcomes among pts with HRMM.
Methods: Thirty-one HRMM patients who achieved stable disease or better were treated beginning at 30-90 days post ASCT with ERd (29/31 pts) or elotuzumab/pomalidomide )/dex (EPd) (2/31 pts) between September 2016 and February 2019. With institutional review board approval, electronic medical records were reviewed for baseline characteristics, treatment history, adverse events (AE) while on therapy as defined by common terminology criteria for adverse events (CTCAE), and survival outcomes. Treatment with ERd or EPd was administered for 4 consecutive 28-day cycles per standard dosing regimens with a tapering or discontinuation of corticosteroids per investigator discretion with cycles 3 and 4. HRMM was defined by any of the following: ISS or Revised-ISS stage 3, CD-138 selected FISH with del 17p, 1q21 gain, t(4;14), t(14;16), and t(14;20), cytogenetics with 13q del or complex karyotype, and/or high-risk gene expression profile score. Ultra-HR pts were defined by having both del 13q and 1q21 gain by FISH based on recent unpublished COMPASS data. Minimal residual disease (MRD) was evaluated upon achievement of very good partial remission or complete remission using 10-color multiparametric flow cytometry. PFS was measured using the log-rank test. Response criteria was defined per International Myeloma Working Group criteria.
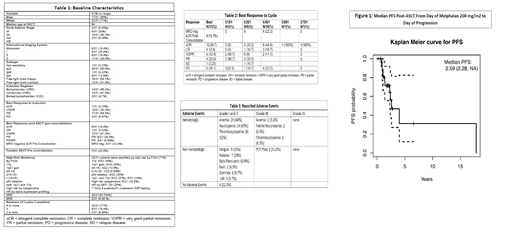
Results: Baseline characteristics of all 31 patients are shown in Table 1. Thirty-four percent were ISS-3, 71% (22/31 pts) had high-risk FISH, of which 19% were ultra-high risk (6/22 pts). Seven pts (22.6%) underwent tandem-ASCT pre-consolidation. Of the 8 pts who had GEP testing, 2 (25%) were high risk. Best response to treatment by cycle is depicted in Table 2. Consolidative ERd/EPd deepened response compared to post-ASCT with 71.4% vs 19.4% achieving stringent complete remission (sCR). Post-consolidation, 19.3% vs 12.9%, pre-consolidation, achieved MRD negativity. With a median follow-up of 24.8 months, median PFS was 31.4 months (Figure 1). There was no significant association between median PFS and variables such as tandem ASCT and ultra-HR using multivariate cox regression. Although all pts experienced at least one AE while on therapy, only 1 patient (3.22%) experienced a grade 3 AE. Hematologic AEs included: anemia (48%), neutropenia (45%), and thrombocytopenia (52%), while the most common non-hematologic AEs included: fatigue (32%), malaise (23%), and back pain (19%). One patient experienced a serious AE (SAE) which was PCP pneumonia requiring hospitalization, resulting in early discontinuation from therapy. There was no treatment-related mortality.
Conclusion: ERd or EPd as 4 months of fixed duration consolidation therapy post-ASCT resulted in a median PFS of 31.4 months amongst pts with HRMM, similar to or perhaps surpassing historical reports of HRMM pts receiving lenalidomide maintenance until progression. This therapy may offer comparable, if not superior, outcomes while having the advantage of allowing for significant time without therapy and perhaps improving quality of life and financial toxicity. This study is limited due to its retrospective nature. Larger prospective studies evaluating fixed duration ERd/EPd in HRMM patients post ASCT should be conducted.
Rowley:Allergan: Equity Ownership; Fate Therapeutics: Consultancy. Goldberg:COTA: Equity Ownership; Bristol-Myers Squibb: Consultancy; Cancer Outcomes Tracking and Analysis (COTA) Inc.: Equity Ownership. Siegel:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Bristol-Myers Squibb Company: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Biran:Bristol Meyers Squibb: Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal