Introduction. Runt-related transcription factor 1 (RUNX1) is a transcription factor critical for normal and leukemic hematopoiesis. Three main isoforms, RUNX1 i-1a, i-1b and i-1c, are produced through alternative splicing of RUNX1. Unlike i-1b and i-1c, i-1a has a Runt homology domain (RHD) but lacks the transactivation domain (TAD), and inhibits transcriptional activity of -1b by competing with higher affinity for target gene sequences. Overexpression of i-1a in cell lines inhibits terminal myeloid differentiation. The i-1a is expressed at high levels in patients (pts) with acute myeloid leukemia (AML). Mutations of RUNX1 are common in CMML and MDS, whereas incidence and clinical correlates of RUNX1 mutations in MPNs are poorly known.
Aim: To analyze the spectrum and clinical correlates of RUNX1 genetic abnormalities (RUNX1-abn), and the expression of RUNX-1a isoform, in a large series of pts with MPNs.
Methods. 686 MPN pts (50 PV, 165 ET, 154 overt-PMF, 143 prefibrotic-PMF, 74 PPV-MF and 100 PET-MF, diagnosed according to 2016 WHO) were included in the study; of these, 625 were analyzed in chronic phase (CP) and 61 at leukemic transformation (LT; of a total of 106 LTs, 58%), including 29 cases with paired samples at diagnosis and LT. Established methods were used for JAK2, MPL and CALR genotyping. A high molecular risk (HMR) category was defined according to Vannucchi A, [Leukemia 2013]. Ion Torrent NGS platform was used to genotype all RUNX1 coding sequence. In 21/29 paired samples, a long reads genome sequencing by Oxford Nanopore technology (ONT) was performed. Copy number variation (CNV) analysis was performed with NanoGLADIATOR package [Magi A, Genome Biol 2019]. Differential expression of RUNX1 mRNA isoform1a and 1b was analyzed by qRT-PCR. Nonparametric Wilcoxon rank-sum test, Kaplan-Meier estimates and log-rank test were used as appropriate.
Results. Somatic RUNX1 mutations were identified in 31 pts (4.5%): 14/625 in CP (2.2%) and 17/61 in LT (27.9%; P<.0001); 7/17 LT pts (41.1%) had two variants. 10/29 paired samples were RUNX1 mutated, in 8 of which mutations were acquired at LT. All mutations were heterozygous (median VAF 40%, range 0.4%-54%); 13 (34.2%) were frameshift, 5 (13.2%) nonsense and 20 (52.6%) missense. Most mutations clustered in RHD (26/38, 68.4%) and TAD (9/38, 23.7%). CNV involving RUNX1 was detected by ONT in 4/21 (19%) paired samples, including 2 gain and 2 loss, all acquired at LT; 2 pts had concurrent RUNX1 mutation. Overall, RUNX1abn, inclusive of mutations and CNV, occurred in 19/61 (31.1%) patients at LT. RUNX1-abn were more common in MPL (12.5%) and TN (7.5%) pts compared with JAK2 (4.3%) and CALR (2.0%) mutated (P=0.04), and were enriched in HMR category (61.3% vs 29.4% vs pts without RUNX1-abn; P=.001). We also analyzed CNV in a total of 47 selected genes included in the RUNX1 pathway (KEGG Orthology K08367); we found CNV in >1 of these genes in 16/21 (76%) pts at LT vs 2/16 (12.5%) of CP pts.
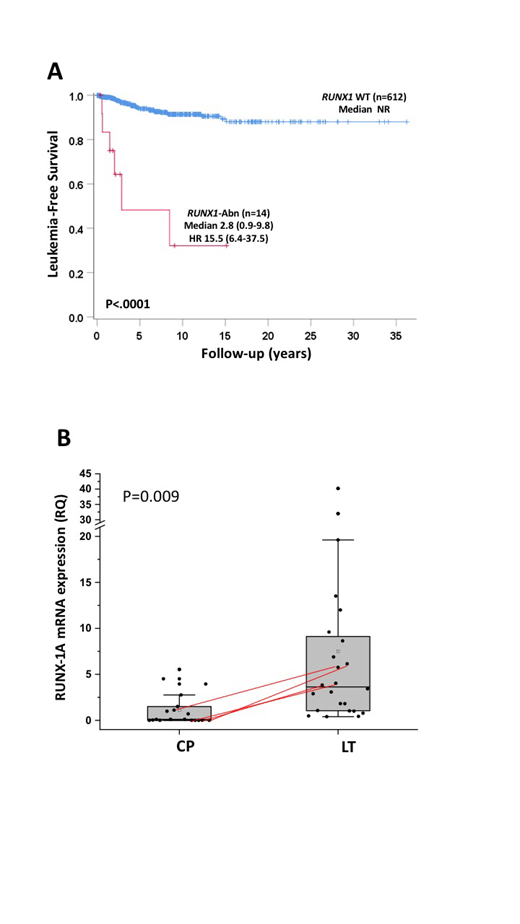
After median follow-up of 4.9y (range 0.1-36.2y) 273 pts died (39.8%). 106 pts (15.4%) progressed to AML after median of 4.7y (0.1-36.2y) from diagnosis. Incidence of LT differed significantly among diseases: 3 pts in PV (5.9%), 17 in ET (10.1%), 39 in overt-PMF (23.5%), 12 in prefibrotic-PMF (8.3%), 11 in PPV-MF (14.1%) and 24 in PET-MF (22.6%). RUNX1-abn were detected, respectively, in 100%, 53.0%, 23.1%, 41.7%, 36.4% and 12.5% of cases at either CP and/or LT. Leukemia-free survival (LFS) was shorter in pts harboring RUNX1-abn in CP compared to RUNX1-WT pt (2.8y vs NR; P<.0001)(Fig 1A).
Expression levels of i-1a and -1b were measured in 34 CP and 24 LT pts. Isoform-1a was significantly elevated in LT pts (mean 7.51±10.1) compared to CP (1.12±1.75; P=.009) (Fig 1B; lines represent the i-1a level rise from CP to LT in 4 paired samples). The i-1a expression levels were irrespective of RUNX1 mutated (mean 7.6±11.9) or unmutated (mean 9.2±6.3) status in LT pts (P=0.8). No difference of i-1b levels in CP (mean 0.9±0.7) versus LP (mean 1.6±1.4; P=0.08) was observed. The expression of i-1a was not dependent on gender, age, leukocyte or platelet count, hemoglobin and percentage of blast cells.
Conclusions. These findings indicate that most MPN pts with LT have involvement of RUNX1 pathway through different mechanisms (mutations, CNV, altered isoform expression, genomic abnormalities of RUNX1 target genes), suggesting that a "RUNX1pathy" may represent a common event during leukemogenesis in MPNs.
Vannucchi:CTI BioPharma: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Italfarmaco: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees; Incyte: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal