Aim:To explore the utility of [18F] Fluoro-2-deoxyglucose (18-FDG) positron emission tomography computed tomography (PET/CT) in lymphoblastic lymphoma (LBL).
Background: LBL is a rare, malignant disorder of precursor T- or B- cells, which forms the lymphoma variant of acute lymphoblastic leukaemia (ALL). Whilst morphologically and immunophenotypically similar to ALL, distinction is made on degree of bone marrow infiltration (typically less than 25% in LBL). Due to the rarity of the condition, investigations at diagnosis, treatment approach and methods to evaluate disease response are not standardised. Bone marrow examination with MRD determination is the gold standard modality for disease monitoring in ALL yet the utility of this investigation is limited in LBL due to the low levels of marrow involvement at presentation. Computed tomography (CT) scanning is widely used in the diagnosis and assessment of lymphomas, however the criteria for disease are based purely on size of a lesion. Difficulties in distinguishing inflammatory from malignant lesions on CT have been widely reported (Elstrom et al. Blood. 2003;101(10):3875-6). 18-FDG PET/CT has been shown to be sensitive for staging high grade non-Hodgkin's lymphoma and is better at differentiating inflammatory from malignant lesions compared to CT alone (Ngeow et al, Ann Oncol. 2009;20(9):1543-7). Normalisation of the SUV to a suitable reference region such as the tumor-to-liver ratio (TLR), has reduced issues with inter-scanner variability. Retrospective data on the use of PET/CT in LBL is limited. In most series, few patients underwent PET/CT at diagnosis making interpretation of subsequent scans difficult thus PET/CT is currently only used at physician discretion in LBL.
Methods: Patients with a diagnosis of T- or B-cell LBL managed at University College London Hospital, a large tertiary haematology unit in the UK since 2011 were identified. Data on timing of PET/CT scans in patients with a diagnosis of LBL were collected retrospectively and correlated with clinical outcome data. SUVmax values within the lesion(s) and within the liver, spleen and mediastinal (aortic) blood pool were collected and the TLR calculated.
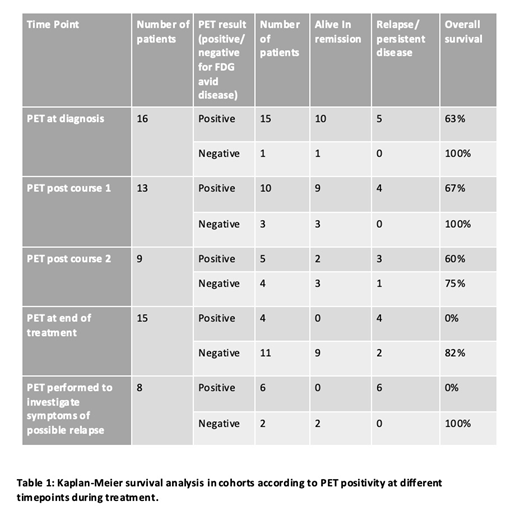
Results:20 patients were identified (14 T-LBL, 6 B-LBL), median age 24.5 years (range 13-66). Ten patients aged 13-24 years were treated using the UKALL 2011 protocol and 10 patients aged >24, years were treated using the UKALL 14 protocol. Sixteen of 20 (80%) of patients had a PET/CT scan at diagnosis before commencing treatment. The remaining 4 patients presented in extremis, requiring intensive care support and immediate empirical treatment. Of the 16 patients who had a PET/CT at diagnosis, all but one had significant FDG avid disease (mean SUVmax 8.6, range 2.7-17.1, TLR >1). Overall survival (OS) for the whole cohort was 70% (median follow up 31 months, range 6-91 months). Consistent with previous published data, OS was superior in the younger patients (90% in the 13-24 year age group vs 50% in those aged >24 years) although due to different patient characteristics and therapy these groups are not comparable. Regardless of age, all patients with a negative PET/CT scan after cycle 1 of chemotherapy survived, disease free (see table 1). Patients with a positive PET/CT after course 2 of treatment or at the end of treatment had a much poorer OS (60% and 0% respectively). In keeping with data from other high-grade lymphomas, SUVmax>10 at presentation may predict an aggressive clinical course, with average SUVmax of 11.9 (TLR4.23) in the patients who died of their disease compared to 6.225 (TLR2.33) in patients who survived. PET/CT had 100% sensitivity and specificity for detecting relapsed disease in this small series. In 8 patients who presented with symptoms suggestive of disease progression or relapse PET/CT detected all 6 patients with true positive disease and excluded relapse in 2 patients with inflammatory lesions.
Conclusions: Our data suggests that PET/CT is useful in the diagnosis and response assessment of LBL particularly if the clinical scenario permits a scan at diagnosis. Although patient numbers are small, these data suggest that a high lesion SUVmax at diagnosis correlates with an aggressive subtype and patients with a negative scan after their first cycle of chemotherapy appear to have an excellent prognosis. Further investigation of the utility of PET/CT in risk stratification in LBL is warranted.
Fielding:Incyte: Consultancy; Pfizer: Consultancy; Amgen: Consultancy; Novartis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal