Background
Treatment options for relapsed or refractory diffuse large B-cell lymphoma (RR DLBCL) represent an unmet medical need. Apatinib is a new oral tyrosine kinase inhibitor mainly targeting vascular endothelial growth factor receptor 2 (VEGFR-2) to inhibit tumor angiogenesis, and has shown encouraging anti-tumor effects in multiple solid tumors. Yet clinical evidence of apatinib as a potential treatment choice for RR DLBCL remains rare. In current study, we evaluated the efficacy and safety of Apatinib for patients with RR DLBCL.
Methods
In this open-label, single-arm, prospective study, we enrolled patients aged 14-70 years with treatment failure of at least two chemotherapeutic regimens using Simon's two stage design. All patients took Apatinib at an initial dose of 500mg on a 4 weeks cycle at home and visited outpatient clinic every 2 cycles to evaluate the efficacy and to record the adverse events. Dose interruptions and reductions were only allowed when there were grade 3 haematological adverse events or grade 2 non-haematological adverse events. We considered objective response rate (ORR) as the primary end point, and progression-free survival (PFS), overall survival (OS) plus duration of response (DoR) as the secondary end point. (This trial was registered at ClinicalTrials.gov, identifier: NCT03376958.)
Results
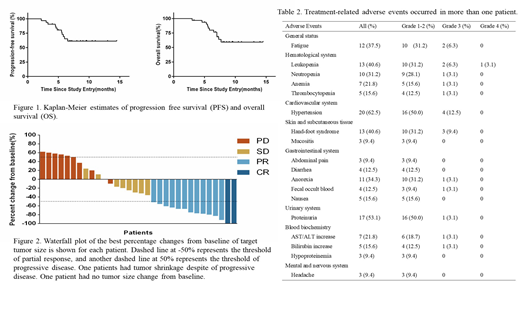
From January 2017 to February 2019, we screened 35 and enrolled 32 eligible patients. At the cutoff point (April 2019), we noted 2 (6.3%) complete responses, 12 (37.5%) partial responses and 9 (28.1%) stable diseases, attributing to an ORR of 43.8% and a disease control rate (DCR) of 71.9%. The median PFS was 6.9 months (95%CI 5.8-7.9) and the median OS was 7.9 months (95%CI 7.0-8.7). Kaplan-Meier estimates of PFS and OS are shown in Figure 1. For patients achieved PR, The median DoR was 5.0 months (95%CI 3.5-6.5). At data analysis time, the median duration of follow-up was 8.6 months (95%CI 7.3-9.4), and 16 (50.0%) patients remained on treatment. 21 patients showed tumor shrinkage comparing with their baseline data and the best percentage changes from baseline are shown in Figure 2. The most common grade 3-4 adverse events (AE) were hypertension (12.6%), hand-foot syndrome (9.4%) and leukopenia (6.3%). No Apatinib-related deaths were noted. AEs arose in at least one patient are shown in Table 1.
Conclusion
With the potential superiority of home administration without frequent hospitalization, apatinib can be an arrow in the bow for RR DLBCL patients considering its favorable efficacy, manageable AEs, improved patient adherence and economic effectiveness. Further investigations into this topic will be of profound significance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal