Cancer initiating cells (CIC) are suggested to be responsible for drug resistance and cancer relapse that are associated with poor prognosis. Therefore, drugs effective for CIC could fulfill an unmet clinical need. We performed a drug screen with chemical libraries to find out new compounds which specifically eradicated CIC established in the previous report (Yamashita et al., Cancer Research, 2015). We obtained compounds with a carboxylic acid skeleton as hit compounds. Interestingly, FF1215T, one of the hit compounds, was shown to inhibit growths of CIC by decreasing intracellular pyrimidine nucleotide levels. Finally, we identified dihydroorotate dehydrogenase (DHODH), which was essential for de novo pyrimidine synthesis as the target of the hit compounds in a ligand fishing assay. FF1215T inhibited DHODH enzymatic activity with the 50% inhibitory concentration value of 9 nM, which showed greater potency than well-known DHODH inhibitors brequinar (12 nM), teriflunomide (262 nM), and vidofludimus (141 nM).
Growing evidence suggests that DHODH is considered to be a promising target to overcome a differentiation blockade of acute myeloid leukemia (AML) cells (Sykes et al., Cell, 2016).Therefore, we explored the effect of FF1215T on AML growth and differentiation. FF1215T demonstrated growth inhibitory effect in multiple human AML cell lines such as U937, MOLM13, HL60, and MV4-11 with the 50% growth inhibition values of 90-170 nM. FF1215T decreased intracellular pyrimidine nucleotide levels, induced DNA damage marker γ-H2AX possibly due to the replication stress, and finally led to apoptosis in HL60 cells. Cell cycle analysis revealed that FF1215T treatment arrested HL60 and THP1 cells at S phase and increased sub-G1 population in these cells. In addition, our DHODH inhibitors induced upregulation of cell-surface CD11b and CD86, which are monocyte and macrophage differentiation markers, morphological changes, and phagocytic activities in several AML cells, indicating differentiation of AML cells toward monocyte and macrophage by DHODH inhibition. FF1215T also depleted UDP-GlcNAc, a substrate for Protein O-GlcNAcylation, and diminished global O-GlcNAcylation and O-GlcNAcylated protein expressions such as c-Myc, SOX2, and OCT4, which play important roles in maintenance and self renewal of stem cells.
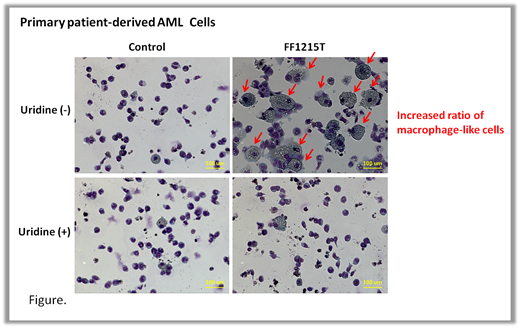
We also found that our DHODH inhibitors induced CD11b and CD86, and increased the ratio of macrophage-like cells in primary patient-derived AML cells and these effects were rescued by uridine supplementation (Fig). Inhibitions of colony formations of primary AML cells were also shown after 14 days of FF1215T treatment. In exploring the value of DHODH inhibitors in the clinic, we identified that our DHODH inhibitors worked to overcome the resistance of standard therapy Ara-C. Our DHODH inhibitors were effective against Ara-C-resistant models of HL60 cells as well as HL60 parental cells. Notably, our DHODH inhibitors synergistically inhibited growths of Ara-C-resistant THP1 cells and enhanced CD11b upregulation of THP1 cells when combined with Ara-C by activating conversion of Ara-C to its active form Ara-CTP.
Next, we optimized the hit compounds and identified an orally available DHODH inhibitor FF14984T that achieved high and prolonged plasma concentrations in vivo. Oral administration of 10 and 30 mg/kg FF14984T once daily for 10 days exhibited significant anti-tumor effects in mice xenografted with HL60 cells. These treatments showed strong reduction of CTP in tumor and induction of DHO in tumor and plasma. When 30 mg/kg FF14984T was orally administrated to orthotropic MOLM13-xenografted mice once daily for 12 days, hCD45+ cells proportions in bone marrow were decreased whereas hCD11bhigh/hCD45+ ratio increased, indicating that FF14984T induced AML differentiation in vivo. Finally, oral administration of 30 mg/kg FF14984T once daily significantly prolonged survival of mice in U937 orthotropic models.
Taken together, we developed a novel potent DHODH inhibitor FF14984T that induced cellular differentiation and anti-leukemic effects on cell lines and primary AML cells. FF14984T is possibly a promising therapeutic option for Ara-C-resistant AML patients that can also benefit from the combination therapy of FF14984T and Ara-C. Identifying the precise mechanism of AML differentiation by DHODH inhibitor and its effects on CIC are currently ongoing.
Kitazawa:FUJIFILM Corporation: Employment. Ishii:FUJIFILM Corporation: Employment. Makita-Suzuki:FUJIFILM Corporation: Employment. Saito:FUJIFILM Corporation: Employment. Takayanagi:FUJIFILM Corporation: Employment. Sugihara:FUJIFILM Corporation: Employment. Matsuda:FUJIFILM Corporation: Employment. Yamakawa:FUJIFILM Corporation: Employment. Tsutsui:FUJIFILM Corporation: Employment. Tanaka:FUJIFILM Corporation: Employment. Hatta:FUJIFILM Corporation: Research Funding. Natsume:FUJIFILM Corporation: Research Funding. Kondo:FUJIFILM Corporation: Research Funding. Hagiwara:FUJIFILM Coporation: Employment. Kiyoi:FUJIFILM Corporation: Research Funding; Astellas Pharma Inc.: Honoraria, Research Funding; Chugai Pharmaceutical Co., Ltd.: Research Funding; Kyowa Hakko Kirin Co., Ltd.: Research Funding; Zenyaku Kogyo Co., Ltd.: Research Funding; Bristol-Myers Squibb: Research Funding; Daiichi Sankyo Co., Ltd: Research Funding; Sumitomo Dainippon Pharma Co., Ltd.: Research Funding; Nippon Shinyaku Co., Ltd.: Research Funding; Otsuka Pharmaceutical Co.,Ltd.: Research Funding; Eisai Co., Ltd.: Research Funding; Takeda Pharmaceutical Co., Ltd.: Research Funding; Pfizer Japan Inc.: Honoraria; Perseus Proteomics Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal