Introduction: Myelodysplastic syndromes (MDS) include a diverse group of bone marrow disorders associated with high mortality and morbidity. In individuals with MDS, the bone marrow produces dysfunctional blood cells with about one-third of patients progressing to acute myeloid leukemia (AML). Previous estimates of the economic burden of MDS are highly variable, with the existing clinical literature deficient of detailed economic data and existing economic studies lacking accurate information on MDS diagnostics. To address the issue, this study uses registry-linked claims data from SEER-Medicare to estimate the economic burden of MDS among elderly individuals in the US.
Methods: We conducted a retrospective case-control study using SEER-Medicare data from January 1, 2010 to December 31, 2016. The study included two cohorts, both aged ≥66 years: (i) patients diagnosed with MDS between January 1, 2011 and December 31, 2015, and (ii) cancer-free controls from a 5% random sample of Medicare beneficiaries. Patients with MDS were followed from index date, defined as the date of initial MDS diagnosis, to death, study end date, or 24 months post-index, whichever occurred first. A 1-year pre-index lookback period was used to identify comorbidities. Except in the instance of death, all individuals had a minimum of 1-year post-index follow-up. We propensity score-matched MDS cases and controls using demographic factors and comorbidities. After examining standardized differences between the MDS and control groups under various caliper widths and allowed numbers of matches, a caliper width of 0.05 of the standard deviation of the propensity score with 25 matched neighbors with replacement was chosen, as this minimized standardized differences across covariates. We calculated average 30-day cost burden for each matched patient based on costs incurred over the number of days in their individual follow-up period. We then estimated incremental healthcare cost burden for patients with MDS relative to the matched controls, including inpatient, outpatient, and pharmaceutical drug costs. We used a generalized linear model (GLM) with a log link and adjusted for demographics and comorbidities.
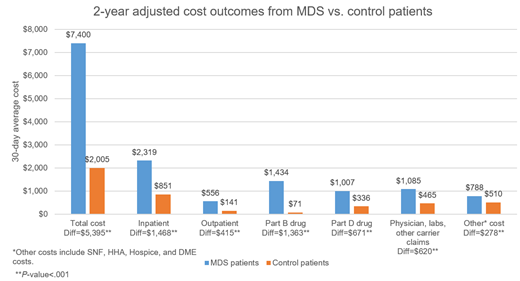
Results: Of the 18,780 patients diagnosed with MDS during the study period, 9,524 met the inclusion criteria. Prior to matching, the control group of 288,877 cancer-free patients was 40% male with a mean age of 75.8 years (SD=8.3), while the MDS group was 57% male with a mean age of 80.1 years (SD=7.4). In addition, standardized differences between the groups were >0.2 for 50% (8/16) of comorbidities considered. After matching, the number of matched controls fell to 109,075 individuals that were 57% male with a mean age of 80.6 (SD=8.4), and standardized differences were <0.04 for all 16 comorbidities. Unadjusted analyses revealed that, in the first two years following diagnosis, patients with MDS had a $6,599/month total cost, $4,005 of which was MDS-related, compared with $2,122/month for matched controls, a difference of $4,478 in total monthly cost (nominal P<.001). After adjusting for patient characteristics using GLM, estimated monthly cost was $7,400/month for patients with MDS and $2,005/month for controls, a difference of $5,395/month (nominal P<.001). This translates to an estimated two-year cost of $177,601 for patients with MDS compared to $48,125 for cancer-free controls, a difference of $129,476. Approximately 58% of this difference was due to higher medical costs, with the remaining 42% due to higher pharmaceutical costs. Higher inpatient hospitalization costs ($2,319/month for patients with MDS; $851/month for controls; $1,468 cost difference, nominal P<.001) and Part B drug costs ($1,434/month for patients with MDS; $71/month for controls; $1,363 cost difference, nominal P<.001) were key drivers of the incremental cost burden.
Conclusion: The economic burden of MDS is higher than that of the cancer-free Medicare population, with an estimated incremental adjusted cost burden of nearly $130,000 in the two years following MDS diagnosis. Medical costs make up the majority of this cost difference. Our results provide an updated estimate of the economic burden of MDS using the most recent data and MDS coding methodology, with detailed estimates of cost by component. Our results fall within the range of estimates of previous studies using SEER-Medicare data.
Shafrin:Precision Medicine Group: Employment, Equity Ownership. Green:Precision Health Economics: Employment, Other: Employee of Precision Health Economics (PHE). PHE received funding from Breath Therapeutics for this research. . Murphy:Precision Medicine Group: Employment. Everson:Precision Medicine Group: Employment. Dennen:Precision Medicine Group: Employment. Price:Jazz Pharmaceuticals: Employment, Equity Ownership. Batt:Precision Medicine Group: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal