<Introduction>
Cord blood transplantation (CBT) has now become one of the alternative stem cell sources for patients with a wide variety of hematological diseases. Considering that cord blood (CB) grafts contain T cells with an immunologically naïve phenotype, concerns have been raised regarding the capability of CB-derived lymphocytes to mediate sufficient graft-versus-leukemia (GVL) effects. However, the incidence of relapse after CBT is reportedly comparable to that after other stem cell sources. Moreover several recent studies have shown even lower relapse rate in CBT compared to the others, despite a lower incidence of GVHD. We and others have reported a unique clinical manifestation, termed pre-engraftment immune reactions (PIR), that develop early after CBT and before engraftment. The unique immune-mediated manifestation may have the potential to cause GVL effect from very early time point after CBT besides GVHD.
<Methods>
We conducted a retrospective study of 551 CB recipients to investigate the GVL effect of the PIR after CBT. Patients who underwent single CBT at our institute from 2004-2017 were included. Only those in non-remission status were included. Patients who had a prior history of allogeneic transplant, who had active infections, who had poor PS, and who received ATG or short-term MTX as GVHD prophylaxis were excluded. The diagnosis of PIR was made when patietns showed a high fever (=>38℃) and at least 2 of the following 5 symptoms (skin eruptions, diarrhea, jaundice, weight gain, and peripheral edema) developed six or more days before neutrophil engraftment. Patients who presented with severe organ damage, such as lung, kidney, or liver dysfunction, were classified as severe type. This study was approved by the institutional review board.
<Results>
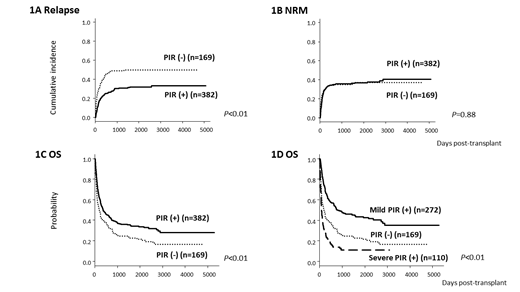
The median age was 57 (range, 16-77) years. All patients had hematological malignancies and all were in non-remission status. Sixty-five percent of these patients received MAC regimens, 63% received tacrolimus plus MMF as GVHD prophylaxis, and 86% received a CB unit with 2 or 3 antigen-mismatch, and the median numbers of TNC and CD34-positive cells were 2.59x107/kg and 0.89x105/kg, respectively. The cumulative incidences of total PIR and severe PIR were 69.3% and 20.0%, respectively, with a median onset of 8 days (range, 5-19) post-CBT. Patients who developed PIR were treated with systemic corticosteroids at the discretion of the primary physicians. Younger age (<55 years) or a lower dose of CD34+ cells were identified as significant factors associated with the development of PIR on univariate analysis, and only younger age was significant on multivariate analysis. Patients with PIR (n=382) showed a significantly lower relapse rate than those without PIR (n=169) (27.2% vs 48.8% at 2 years, P<0.01), while there was no major difference in the non relapse mortality (NRM) rate between the two groups (35.7% vs 34.9% at 2 years, P=0.88) (Figure 1A and 1B). Patients with severe PIR (n=110) showed a more pronounced decrease in relapse incidence (12.5% in severe PIR group vs 33.1% in mild PIR group vs 48.8% in PIR (-) group, P<0.01). The cumulative incidence of NRM in the group, however, was extremely high compared to the others (73.3% in severe PIR group vs 20.8% in mild PIR group vs 34.9% in PIR (-) group, P<0.01). Patients with mild PIRs (n=272) showed reductions of both relapse and NRM compared to those without PIRs. The lower incidence of relapse in the PIR group was translated to better 2-year overall survival (OS) compared to those without PIR (41.2% in PIR (+) group vs 31.5% in PIR (-) group, P<0.01) (Figure 1C). Two-year OS of those with mild PIR was better than the other 2 groups (52.0% in mild PIR group vs 31.5% in PIR (-) group vs 13.9% in severe PIR group, P<0.01) (Figure 1D). Patients with severe PIR showed worse OS, mainly due to the higher incidence of NRM. A higher GVL effect was observed in patients with myeloid malignancies than in those with lymphoid malignancies.
<Conclusions>
Our data clearly showed that development of PIR after single CBT reduces relapse rate without increasing NRM and contributes to superior survival rate in advanced hematological malignanicies. PIR is one of the clinically important factors associated with unique GVL effects after single CBT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal