Introduction: Predictors routinely used to assess long-term survival after allogeneic hematopoietic cell transplantation (alloHCT) have not been specifically validated for pre-transplant risk assessment of patients getting cord blood transplantation supported by Haplo-CD34+ Progenitor cells as a myeloid bridge (haplo-cord).
Methods: All consecutive adult patients with hematological malignancies who received an alternative donor alloHCT with a haplo-cord at Weill Cornell Medicine were included. Data was collected from an ongoing haplo-cord protocol (clinicaltrials.gov identifier 01810588). Plasma cell disorders were excluded. Age, CIBMTR Disease Risk Index (DRI), Karnofsky performance score (KPS), and HCT comorbidity index (HCT-CI) (routinely calculated since 06/2014), were assessed before alloHCT. The Kaplan-Meier method was used to estimate OS probabilities. Comparisons of OS were evaluated by the log-rank test. Significant predictors were considered in a Cox proportional hazards regression model using forward stepwise selection. A cumulative incidence function (CI) for relapse was calculated using a competing risk model for non-relapse mortality (NRM). We further validated our findings in the subgroup of patients with AML.
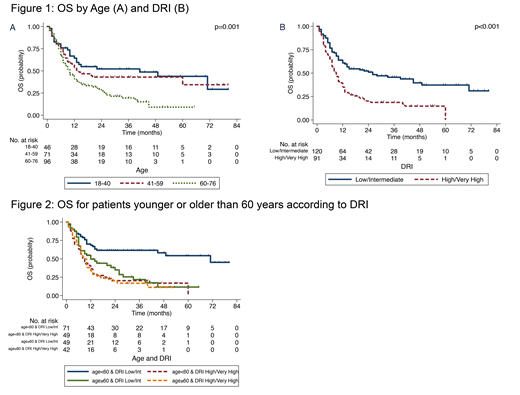
Results: Between 06/2012 and 12/2018, 217 patients underwent haplo-cord transplantation. Indications for alloHCT included: 66% leukemia, 19% MDS/MPN, 15% Lymphoma. Median age was 58 yr (22% ≤ 40yrs, 33% between 41-59yrs, and 45% ≥ 60 yrs). 43% of patients were women. KPS score was ≥ 90 in 56%. DRI was high/very-high in 43% and low/intermediate in 56%. HCT-CI for 154 patients was 0 in 14%, 1-2 in 21%, 3-5 in 45% and ≥ 6 in 20%. Conditioning regimens included fludarabine with melphalan 45%, plus TBI 51%, other 4%. Median follow-up was 30 months. 2yr OS was 38% (95%CI 31-44%). 2yr CI of NRM was 35% and relapse 36%. Age (p=0.001), DRI (p<0.001), and KPS (p=0.003) were associated with OS in univariate analysis(Figure 1). HCT-CI did not correlate with OS (p=0.53). In a multivariable model, only age ≥60 (HR 1.86, p=0.01) and high/very high DRI (HR 1.86, p<0.001) remained predictive of OS. (Figure 2). Age ≥ 60 was associated with increased NRM at 2 yrs (45% vs 27%, p=0.01). High/very high DRI was associated with relapse at 2 years (51% vs 24%, p<0.001). A subgroup analysis of 123 patients with AML showed consistent findings; age ≥ 60 (HR 2.11, p=0.04) and high/very high DRI (HR 2.51, p<0.001) remained predictive for OS in multivariable analysis.
Conclusion: DRI and age are highly predictive of OS for patients undergoing haplo-cord transplantation. Our finding that HCT-CI is not predictive of OS when applied to haplo-cord alloHCT is supported by previous findings investigating the role of HCT-CI in cohorts with cord blood donors (Adachi Y et al BBMT 2018 and Majhail N et al BBMT 2008). To this end, our findings demonstrate that a high HCT-CI score should not preclude patients from evaluation for alternative donor transplantation using cord blood supported by Haplo-CD34+ progenitor cells. Other prognostic tools to assess specific comorbidities impacting this transplant platform are needed for accurate pre-transplant risk assessment in order to improve decision making and clinical trial assignments.
Van Besien:Miltenyi Biotec: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal