Background: Although allogeneic hematopoietic stem cell transplantation (allo-HSCT) can provide sustained remission for adult T-cell leukemia/lymphoma (ATL), its prognosis is still unsatisfactory. Alternative donor sources are often utilized in allo-HSCT for ATL, but advantages and disadvantages of each donor source have not been fully elucidated. Graft-versus-host disease (GVHD) -free, relapse-free survival (GRFS) has been proposed as a novel and clinically meaningful endpoint of allo-HSCT. Whereas GVHD has been relatively accepted in ATL to induce substantial graft-versus-tumor (GVT) effects, severe GVHD is associated with non-relapse mortality and disturbs quality of patients' life. Analyses of GRFS may illustrate important aspects to optimize the balance between regulating GVHD and enhancing GVT effects in ATL patients.
Patients and methods: We retrospectively analyzed the data of 1363 patients with ATL who received first allo-HSCT from 2006 through 2015 in Japan. Data were collected from the nationwide database maintained by the Japan Society of Hematopoietic Cell Transplantation. The probability of OS and GRFS was estimated according to the Kaplan-Meier method, and univariate comparisons among the groups were performed using the log-rank test. The Cox proportional hazard model was used for the multivariate analysis of OS and GRFS.
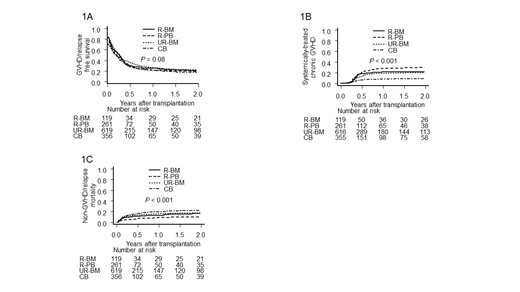
Results: Median age was 57 years-old (range: 20-78) and median observation period of survivors was 3.1 years (range: 0.0-10.5). One-year OS and GRFS were 45% and 24%, respectively. OS of cord blood transplantation (CB) (37% at 1 year, n = 359) was worse than those of related bone marrow transplantation (R-BM) (48%, n = 121), related peripheral blood stem cell transplantation (R-PB) (50%, n = 264) and unrelated bone marrow transplantation (UR-BM) (47%, n = 619) (p < 0.001). However, in the cases of complete remission (CR) at allo-HSCT, OS of CB (n = 132) was 52% at 1 year and not inferior to those of R-BM (54%, n = 52), R-PB (57%, n = 88) and UR-BM (58%, n = 280) (p = 0.14). The cumulative incidence of relapse in CB was 47% at 1 year and higher than those of R-BM (40%), R-PB (43%) and UR-BM (35%) (p = 0.002). However, in CR cases, the cumulative incidences of relapse were lower in UR-BM (21% at 1 year) and CB (26%) than those in R-BM (31%) and R-PB (31%), though not significant (p = 0.21). Notably, there were no significant differences in GRFS of CB, R-BM, R-PB and UR-BM (21%, 25%, 21% and 26% at 1 year, p = 0.08, Figure 1A). It was attributed to low incidence of chronic GVHD which needed systemic therapy in CB (9% at 1 year, R-BM: 22%, R-PB: 28% and UR-BM: 18%, p < 0.001, Figure 1B) and low incidence of non-GVHD/relapse mortality in R-PB (9% at 1 year, CB: 20%, R-BM: 13% and UR-BM: 16%, p < 0.001, Figure 1C). In R-BM and UR-BM, there were no significant differences as for OS and GRFS between HLA-matched and HLA-mismatched transplantations. In R-PB, OS of HLA haploidentical transplantation (Haplo, n = 36) was 39% at 1 year and tended to be inferior to those of HLA 6/6-matched (53%, n = 183) and HLA 5/6-matched transplantation (49%, n = 45) (p = 0.11). There was no significant difference as for GRFS among these 3 groups (Haplo: 22%, 6/6-matched: 20%, 5/6-matched: 27% at 1 year, p = 0.69). Finally, multivariate analysis revealed that male sex, higher age (> 50 years), worse PS (> 1) and non-CR at allo-HSCT were associated with lower OS and GRFS. Importantly, donor sources and HLA mismatch were not associated with OS and GRFS.
Conclusions: Our results imply that all donor sources are feasible for CR cases and can be selected depending on their clinical characteristics such as frailty and history of infection. While the main issue of CB is high non-GVHD/relapse mortality, it is warranted to suppress severe GVHD in R-PB. Thus, GRFS provides important clues to improve the outcome of allo-HSCT for ATL.
Shindo:Novartis: Research Funding. Nakano:Novartis: Honoraria. Ichinohe:Astellas Pharma: Research Funding; Chugai Pharmaceutical Co.: Research Funding; CSL Behring: Research Funding; Eisai Co.: Research Funding; Kyowa Hakko Kirin Co.: Research Funding; Ono Pharmaceutical Co.: Research Funding; Pfizer: Research Funding; Nippon Shinyaku Co.: Research Funding; MSD: Research Funding; Otsuka Pharmaceutical Co.: Research Funding; Repertoire Genesis Inc.: Research Funding; Sumitomo Dainippon Pharma Co.: Research Funding; Taiho Pharmaceutical Co.: Research Funding; Takeda Pharmaceutical Co.: Research Funding; Zenyaku Kogyo Co.: Research Funding; Alexion Pharmaceuticals: Honoraria; Bristol-Myers Squibb: Honoraria; Celgene: Honoraria; JCR Pharmaceuticals: Honoraria; Janssen Pharmaceutical K.K.: Honoraria; Mundipharma: Honoraria; Novartis: Honoraria. Atsuta:CHUGAI PHARMACEUTICAL CO., LTD.: Honoraria; Kyowa Kirin Co., Ltd: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal