Background: The use of unmanipulated Haploidentical HSCT (Haplo-HSCT) with post-transplant Cyclophosphamide (PT-Cy) as GVHD prophylaxis has widely extended. Veno-occlusive disease (VOD) is a threatening complication after both autologous and allogeneic HSCT, with high mortality rates despite early medical treatment, including the use of defibrotide. The objective of this study was to describe characteristics and outcomes of patients with refractory very severe VOD after Haplo-HSCT with PT-Cy, treated with TIPS as salvage procedure.
Methods: We retrospectively analysed 176 Haplo-HSCT with Cy-post consecutively performed between 2011 and May 2019 in a single centre. VOD was defined according to modified Seattle, Baltimore or revised EBMT criteria. Severity was retrospectively graded according to revised EBMT severity criteria into four categories: mild, moderate, severe and very severe. Complete response (CR) was defined as a normal total bilirubin level (<2 mg/dL) or, in patients with normal bilirubin or alternative causes of hyperbilirubinemia, as normalized renal function, reduction of elevated transaminase level <50%, tense ascites resolution, and no need for oxygen supplement in the absence of alternative hypoxemia causes.
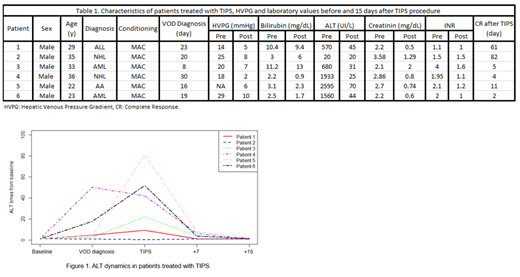
Results: Sixteen patients (9.1%) met the modified Seattle, Baltimore or revised EBMT diagnostic criteria for VOD. Ultrasound with Doppler ultrasonography was performed in all patients, and at least indirect signs of VOD were found in all cases. Based on revised EBMT severity criteria, there were 2 mild (12.5%), 2 moderate (12.5%), 2 severe (12.5%) and 10 very severe (62.5%) grade VOD. Twelve patients (75%) were treated with defibrotide, including all patients with very severe VOD, except one with CNS hemorrhage (Patient 1). Six patients with very severe VOD, were treated with TIPS due to rapid clinical or analytical deterioration or refractory hepatorenal syndrome, despite medical treatment including defibrotide (Table 1). All were male patients, with a median age of 31 years (range 22-36), all transplanted with myeloablative conditioning regimen. TIPS insertion was performed on a median time since VOD diagnosis of 5 days (range 1-28) without technical complications in any case. Median total bilirubin, ALT, creatinine and INR the day of procedure were 3 mg/dL (range 2.2-11.2), 1120 UI/L (range 10-2595), 2.45 mg/dL (range 2.06-3.58) and 1.96 (range 1.1-4) respectively. Median hepatic venous pressure gradient (HVPG) prior to and after TIPS was 22.5 (range 14-29) and 6.5 (range 2-10) mmHg respectively, with a median drop of 16.5 mmHg (range 9-19). Following TIPS, all patients showed clinical improvement with hepatomegaly, ascites and renal failure resolution, and all showed analytical improvement with bilirubin, creatinine and ALT values reduction, except for patient 2, whose TIPS indication was refractory hepatorenal syndrome with normal ALT levels (Figure 1). The 5 patients who had iniciated defibrotide before TIPS, completed 21 days of treatment. All patients met criteria for CR in a median of 8 days after TIPS insertion (range 2-82). The 100-day overall survival (OS) was 100%. Five patients were alive with normal liver and renal function at last follow up, and one patient died due to infection 7 months after Haplo-HSCT, with VOD in complete resolution.
Conclusions: Incidence of VOD after Haplo-HSCT with PT-Cy is comparable to those reported after HLA-identical HSCT series. Most of the patients developed very severe VOD according to revised EBMT severity criteria. For patients with rapid progressive VOD, early TIPS insertion allowed completion of defibrotide therapy. The use of TIPS together with defibrotide resulted in complete response and no associated complications with a 0% of VOD associated mortality in spite of high severity. ALT values may be the best predictor of CR after TIPS procedure. In our experience, timely and individualized use of TIPS significantly improves outcome of very severe VOD after Haplo-HSCT. Therefore, TIPS should be promptly considered in rapid progressive cases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal