The identification of risk factors for progression is critical in the clinical management and appropriate follow up of patients with pre-malignant Asymptomatic Monoclonal Gammopathies (AMG) including Monoclonal Gammopathy of Undetermined Significance (MGUS) and Smoldering Multiple Myeloma (SMM). The development of prognostic score and consequently the early identification of patients with possible short-term progression to Multiple Myeloma (MM) could lead to anticipate the treatment.
In this study, we retrospectively evaluated possible risk factors of short-term progression to active MM in a large cohort of MGUS and SMM patients admitted to a single haematological center (Hematology and BMT Unit, University Hospital of Parma) between 2010 and 2018. We analysed a total cohort of 235 patients diagnosed with AMG (81 MGUS and 154 SMM) according to the IMWG recently updated diagnostic criteria. All patients analysed underwent to Bone Marrow (BM) examination; moreover, imaging evaluation was performed in 22 MGUS and 123 SMM patients, in order to exclude the presence of bone disease. In a subgroup of AMG patients (n=50), bone mineral density (BMD) evaluation by Dual-energy X-ray Absorptiometry (DXA) was also available.
Median age of the AMG patients analysed was 68 years (range 35-93 years). Median percentage of BM plasma cells (BMPCs) was 12% (range 2-55%) in the entire population, 7% (range 2-9) in MGUS and 15% (range 10-55) in SMM patients. Median serum M-protein was 1.7 g/dL (range: 0.17-4.5), 1.5 g/dL (range 0.17-4.5) in MGUS and 1.8 g/dL (range 0.4-2.7) in SMM patients. An abnormal free light chain (FLC) ratio was found in 70% of AMG patients, among the ones that performed the analysis; regarding SMM patients, FLC ratio value was available in 97 patients: in 72 (76%) the ratio was unbalanced, 37 (39%) had a FLC ratio ≤ 0.125 or ≥ 8 and in 14 (15%) it was > 20; among MGUS patients, value was collected in 41 patients and in 21 (51%) it was <0.26 or >1.65. The presence of immunoparesis in one or two uninvolved immunoglobulins occurred in 59% of the entire population.
The median follow up time was 18 months (range 0 - 111 months) for whole population. Overall 44 patients of the entire cohort progressed to MM (41 SMM and 3 MGUS) with a median TTP of 14.5 months.
By univariate analysis we found that percentage of BMPCs, entity of M-protein and presence of immunoparesis were significantly correlated with progression to active MM (p<0.001 for each variable). On the other hand, abnormal FLC ratio did not reach a statistical significance, as well as value of the involved FLC (p=0.059). Nevertheless, the presence of a FLC ratio < 0.125 or > 8 (as used in Mayo scoring system for SMM) showed a relationship at the limit of statistical significance in this subgroup of patients (p=0.052). Any significant correlation was not observed with age, sex, Ig isotype, light chain's type and the BMD values (p=NS).
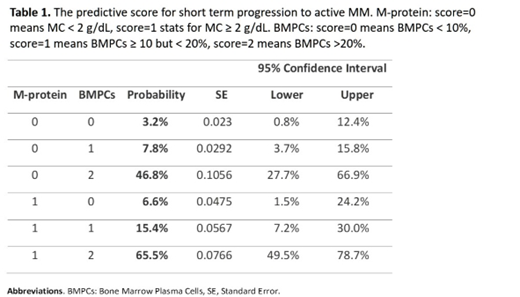
Afterwards, we applied Kaplan Meier method on risk factors resulted significant in univariate analysis demonstrating that they also significantly influenced the time to progression to MM. Finally, through a binomial logistic regression, we developed a new prognostic score for whole population. By combining the values of M-protein (< 2, score=0 or ≥ 2 g/dL, score=1) and the percentage of BMPC (<10%, score=0, 10-20%, score=1 and >20%, score=2), we obtained six groups at different probability of progression to active MM (Table 1). Given that result, we stratified patients in 3 groups: low-risk (score=0), intermediate-risk (score=1) and high-risk (score≥2); log-rank test confirmed that high-risk patients had a significantly shorter time to progression to symptomatic MM as compared to intermediate and low-risk patients (p<0.001).
In conclusion, our results show that in patients with AMG the clinical factors, which mostly impact on the short-term risk of progression to active MM, are the entity of the PCs infiltrate and the MC related to the tumoral mass. The development of a clinical score based on BMPCs and M-protein will permit to overcome the traditional distinction between MGUS and SMM in the evaluation of the progression of AMG patients to active MM.
Giuliani:Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal