Introduction:
The Bruton's Tyrosine Kinase (BTK) inhibitor ibrutinib (IB) is a standard therapy for previously untreated CLL patients. While therapy is currently indicated only for patients with progressive, symptomatic disease, the introduction of targeted therapies in CLL has re-opened the question of whether asymptomatic high risk patients would benefit from early intervention. As well, even in early stages CLL is associated with profound cellular, humoral and innate immune suppression and patients with CLL respond poorly to routine vaccinations. IB has been shown to reverse disease mediated immune dysfunction partly through Th1 skewing. We undertook a phase 2 study of IB in asymptomatic high risk CLL patients who did not otherwise require therapy to evaluate: 1) the safety and efficacy of 2 years of IB in this clinical setting and 2) ability of IB to improve the efficacy of routine vaccines.
Methods:
This is a single-stage phase II study of IB in previously untreated asymptomatic, genetically high-risk patients with CLL, who did not meet IWCLL treatment criteria. High risk genomics were defined as del(11)(q22.3), del(17)(p13.1), unmutated IGHV, and/or complex karyotype (≥3 cytogenetic abnormalities). Patients were randomized to receive IB 420mg PO daily either concurrent with the pneumococcal (PCV13), influenza and TdaP vaccines (Arm A) or following vaccination (Arm B) for a total of 27 cycles (2 years). The primary objective of the study was to determine the safety and 2-year progression-free survival (PFS) of asymptomatic, high-risk CLL patients treated with IB. Secondary objectives include determination of safety and immune responses to vaccines in relation to IB administration, development of resistance, and quality-of-life (QOL). QOL measures assessed general QOL (SF-12, EORTC), anxiety (GAD-7) and depression (PHQ-9).
Results:
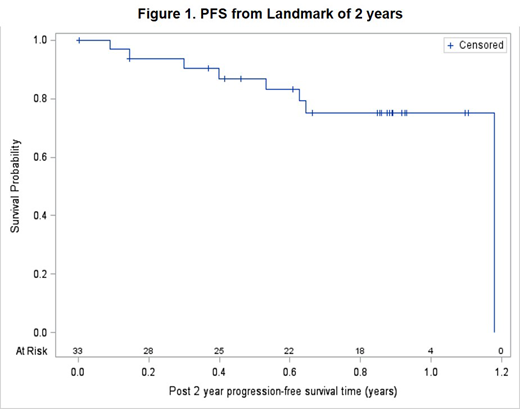
Forty-four patients (pts; 21 in Arm A, 23 in Arm B) were enrolled from 1/2016 to 6/2017, with a median age of 58 (range 35-82). Sixty-six percent of pts were male and all were high-risk: 91% with unmutated IGHV, 14% with del(17)(p13.1), 34% with del(11)(q22.3), and 24% with complex karyotype (≥ 3 abnormalities). Median follow-up is 2.6 years (range: 0.2-3.2). Excluding 2 patients in Arm B who progressed prior to receipt of IB, 2-year PFS was 92%. From a landmark of 2-years and including 33 patients who reached this point and discontinued IB, 6-month PFS was 87% (95% CI: 69-95%; Figure 1). Of 9 pts who progressed after IB discontinuation, 3 have not required further treatment, 5 restarted IB or acalabrutinib, and 1 started venetoclax/rituximab, and all responded. For PCV13, in Arm A, 15/16 patients showed a significant increase in antibody titer 2 cycles following vaccination, but response disappeared by cycle 12. In Arm B, 3/13 patients had an increase in antibody titer, with no increase following second vaccination. For influenza, patients in Arm B showed a significant response to influenza A vaccination, while patients in both arms responded to influenza B vaccination.
IB was generally well tolerated, and only one pt discontinued treatment due to toxicity (atrial fibrillation). Grade 3+ toxicities that occurred in >2% of patients included anemia (7%), atrial fibrillation (11%), dental caries (7%), hyperglycemia (7%), hypertension (43%), and neutropenia (7%). At baseline, patients' reports of physical health-related (M=48.52, SD=7.96) and mental health-related quality of life (M=52.20, SD=8.57) similar to U.S population norms, along with moderately high global health (M=78.49 of 100, SD = 20.51). Additionally, patients' anxiety (M=3.56, SD=4.71) and depressive symptom reports (M=3.65, SD=4.46) were in the "none/mild" range. There was no significant change in the latter measure from baseline to 12 months (p>0.25), excepting anxiety which slightly decreased (M=1.31, SD=2.33; F(3,44)=5.94, p<0.01).
Conclusions
Early intervention with IB was well tolerated and significantly improved patient disease status. Vaccine response to PCV13 was improved by concurrent ibrutinib, but lost at 12 months, suggesting re-vaccination might be helpful. Quality of life remained good throughout treatment, with improvement in patient anxiety. Extended follow-up will be required to determine how long remissions can be maintained after drug discontinuation in this population.
Woyach:Verastem: Research Funding; Loxo: Research Funding; Morphosys: Research Funding; Karyopharm: Research Funding; AbbVie: Research Funding; Janssen: Consultancy, Research Funding; Pharmacyclics LLC, an AbbVie Company: Consultancy, Research Funding. Rogers:AbbVie: Research Funding; Acerta Pharma: Consultancy; Genentech: Research Funding; Janssen: Research Funding. Bhat:Pharmacyclics: Consultancy; Janssen: Consultancy. Grever:Acerta Pharma, LLC: Membership on an entity's Board of Directors or advisory committees. Lozanski:Beckman Coulter: Research Funding; Stemline Therapeutics Inc.: Research Funding; Boehringer Ingelheim: Research Funding; Genentec: Research Funding. Byrd:TG Therapeutics: Other: Travel Expenses, Research Funding, Speakers Bureau; Acerta: Research Funding; Novartis: Other: Travel Expenses, Speakers Bureau; Gilead: Other: Travel Expenses, Research Funding, Speakers Bureau; Ohio State University: Patents & Royalties: OSU-2S; Janssen: Consultancy, Other: Travel Expenses, Research Funding, Speakers Bureau; Genentech: Research Funding; BeiGene: Research Funding; Pharmacyclics LLC, an AbbVie Company: Other: Travel Expenses, Research Funding, Speakers Bureau. Awan:Gilead: Consultancy; Sunesis: Consultancy; Pharmacyclics: Consultancy, Research Funding; AstraZeneca: Consultancy, Speakers Bureau; Abbvie: Consultancy, Speakers Bureau; Janssen: Consultancy; Genentech: Consultancy.
Clinical trial of ibrutinib used in an off-label setting
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal