Introduction: The BTK inhibitor ibrutinib is used as first line of therapy (LOT) and salvage therapy in CLL patients and in combination with chemotherapy, anti-CD20 biologics, and venetoclax among other drugs. Several studies have shown that 10-20% of patients receiving ibrutinib discontinue due to intolerance, disease progression, transformation, or other causes. Those who discontinue due to disease transformation or early disease progression are reported to have increased mortality risk. This study was conducted to provide much-needed RWD on CLL treatment patterns and treatment-related AEs.
Methods: CLL patients first diagnosed between 2012 and 2019 were identified in a 200 million patient claims/EHR dataset. All patients were aged 18+, had two claims for CLL submitted at least 1 week apart, and were treated with an antineoplastic medication following diagnosis. All patient characteristics were defined using ICD-9/10, CPT, RxNorm, and LOINC codes.
To examine treatment patterns, the start date of the first LOT was defined as the time of the first treatment following the CLL diagnosis. All medications taken within 28 days of the start date were grouped into a combination LOT. The second and subsequent LOTs started when a new medication was identified in a patient's record or when 365 days passed without any record of a medication. Time on treatment was defined as the number of months between the first and most recent record of an ingredient in a patient's EHR.
ED was defined as any patients who discontinued their first antineoplastic within the first month after the initial CLL diagnosis. The frequency of diagnoses in the month before discontinuation were used to examine potential reasons for discontinuation among the two largest treated populations: patients treated with ibrutinib and patients treated with rituximab and bendamustine (rit+bend). Patients who discontinued therapy were compared to patients who continued with therapy (continuers), using the first treatment recorded in the month after diagnosis as the index date in both groups, and adjusting for demographics using a 1:1 matched propensity score model. Following the index event, a Kaplan-Meier analysis measured the event-free survival probability for anemia, transfusions, and all-cause mortality.
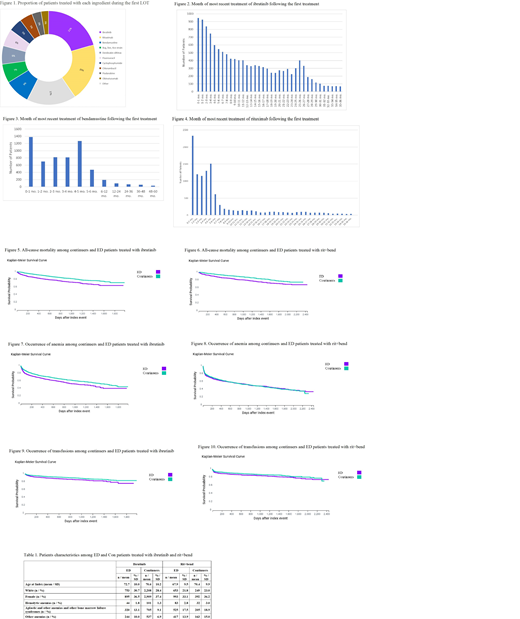
Results: The mean age at diagnosis of the 38,653 CLL patients identified in the dataset was 70.4 (+10.7). In the first LOT, 67 unique ingredients were identified. The most common medications included ibrutinib (21%), rituximab (20%), bendamustine (9%), fluorouracil (6%), cyclophosphamide (5%), chlorambucil (5%), and fludarabine (3%) (Fig 1). Most patients were treated with a single LOT and did not progress to other medications. Among patients who progressed from ibrutinib in the first LOT, other antineoplastics made up the most common second LOT. Patients with an antineoplastic recorded in the first LOT were more likely to switch to ibrutinib than any other therapy. Patients treated with a combination of rit+bend most often switched to ibrutinib or other antineoplastics as a second LOT.
Patients treated with ibrutinib remain on treatment for longer than patients treated with rituximab and bendamustine. Among patients treated with ibrutinib, the length of treatment decreased monotonically over two years (Fig 2). The proportion of patients treated with rituximab dropped off substantially after 6 months (Fig 4).
In the month before the index treatment, ED patients treated with ibrutinib had a higher prevalence of anemia, pain, and malaise/fatigue as compared to continuers. Among rit+bend patients, characteristics were similar between continuers and ED patients (Tab 1). Among both ibrutinib and rit+bend treated patients, continuers had a higher survival probability than ED patients (p<0.05) (Fig 5 and 6). Continuers treated with ibrutinib were less likely to develop anemia and receive a transfusion (p<0.05) (Fig 7 and 9).
Conclusions: The treatment landscape in CLL includes many off-label therapies including monoclonal antibodies and other chemotherapies. However, most patients remain on either ibrutinib or rit+bend for the length of care. Patients who do not discontinue a therapy within the first month are less likely to develop complications and have a lower probability of all-cause mortality. Further research is needed to understand the dynamics of more complex treatment pathways.
Kuranz:TriNetX, Inc: Employment. Stacey:TriNetX, Inc: Employment. Luciano:TriNetX, Inc: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal