Background: Relapsed or refractory (R/R) transformed indolent B-cell non-Hodgkin lymphoma (iB-NHL) is an uncommon clinical entity associated with poor prognosis. Unfortunately, most trials of aggressive B-NHL tend to specifically exclude transformed disease resulting in scant prospective data to guide therapy. We performed a prospective phase II trial of single agent ibrutinib in patients with previously treated transformed iB-NHL and now report the final results (NCT02207062).
Methods: Eligibility included measurable, biopsy-proven transformed iB-NHL, no prior ibrutinib, ECOG 0-2, and prior receipt of ≥ 1 line of therapy for the transformed disease. Treatment consisted of oral ibrutinib 560 mg daily until disease progression or unacceptable toxicity. The primary endpoint was investigator-assessed overall response rate (ORR, per Lugano criteria by independent radiology review), with a predefined threshold of success ≥ 30%. Secondary endpoints included clinical benefit rate (CBR, defined as ORR and/or stable disease of ≥ 6 months), progression-free survival (PFS), overall survival (OS), and safety. Exploratory endpoints included ORR according to cell-of-origin (COO) of transformed lymphoma assessed by Hans algorithm and disease burden measured by computed tomography (CT) and metabolic tumor volume (MTV).
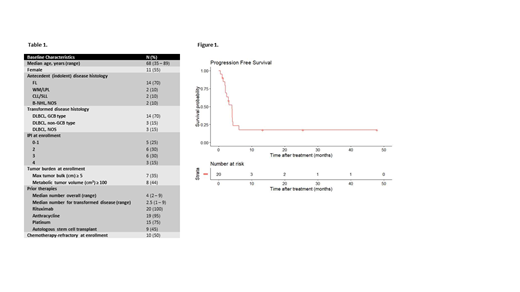
Results: From October 2014 to March 2019, 20 patients were treated (Table 1). At enrollment, patients had received a median of 4 prior therapies (range 2 to 9) and were refractory to chemotherapy in 10 (50%) cases. Histology of transformed disease was diffuse large B cell lymphoma (DLBCL) in all patients. Two patients came off study prior to response assessment and without clinical evidence of disease progression: 1 after 1.3 months for intractable mucositis and 1 who died suddenly and without known cause 1.9 months into treatment.
Median time on therapy was 3.1 months range (0.6 to 48.0) with 3 (15%) patients continuing on therapy > 1 year. Eighteen patients were evaluable for response. The ORR was 39% (complete response = 17%) and CBR was 44%. Median PFS and OS were 4.1 and 22.4 months, respectively, and median duration of response was 2.3 months; estimated 12-month PFS was 18% (Figure 1). ORR was more common in cases of low tumor burden but this association did not meet statistical significance on univariate analysis (p = 0.15 for maximum tumor < 5 cm by CT and p = 0.06 for MTV < 100 cm3). ORR was superior after prior autologous hematopoietic stem cell transplantation (auto-HSCT) (p = 0.01) and was not associated with DLBCL COO (p = 0.75).
Dose holds for toxicity were required on 6 occasions in 5 (25%) patients for a median duration of 17.5 days (range 8 to 21); no reductions in dose were performed. Ibrutinib was resumed after resolution of toxicity at full dose in each case with the exception of an episode of pneumonia that, despite resolution, prompted the patient to stop treatment on study. Adverse events (AEs) considered related to ibrutinib were most commonly grade 1-2 and included fatigue (55%), bruising (55%), and diarrhea (35%). Grade ≥ 3 AEs included atrial arrythmia in 2 patients and the following AEs in 1 patient each: ventricular arrythmia, neutropenia, lymphopenia, mucositis/esophagitis, nausea, pneumonia, sepsis, and death of unknown cause.
Conclusions: Ibrutinib appears active in R/R transformed iB-NHL and may provide extended disease control for a subset of patients or as part of a bridging strategy prior to CAR-T or transplant. The observed toxicity profile was consistent with other trials. Efficacy may be greater in cases of lower tumor burden and in patients previously treated with auto-HSCT. Further investigation of ibrutinib and focused study of agents in transformed iB-NHL is warranted.
Graf:BeiGene: Research Funding; AstraZeneca: Research Funding; TG Therapeutics: Research Funding. Cassaday:Pfizer: Consultancy, Honoraria, Research Funding; Incyte: Research Funding; Kite/Gilead: Research Funding; Merck: Research Funding; Seattle Genetics: Research Funding; Seattle Genetics: Other: Spouse's disclosure: employment, stock and other ownership interests; Amgen: Consultancy, Research Funding. Lynch:Rhizen Pharmaceuticals S.A: Research Funding; Incyte Corporation: Research Funding; Takeda Pharmaceuticals: Research Funding; T.G. Therapeutics: Research Funding; Johnson Graffe Keay Moniz & Wick LLP: Consultancy; Juno Therapeutics: Research Funding. Krakow:Bellicum Pharmaceuticals: Research Funding; Highpass Bio: Research Funding; Magnolia Innovations: Consultancy. Smith:Denovo Biopharma: Research Funding; Acerta Pharma BV: Research Funding; Portola Pharmaceuticals: Research Funding; Incyte Corporation: Research Funding; AstraZeneca: Membership on an entity's Board of Directors or advisory committees, Research Funding; Genentech: Research Funding; Bristol-Myers Squibb (spouse): Research Funding; Ignyta (spouse): Research Funding; Ayala (spouse): Research Funding; Pharmacyclics: Research Funding; Merck Sharp & Dohme Corp: Consultancy, Research Funding; Seattle Genetics: Research Funding. Gopal:Seattle Genetics, Pfizer, Janssen, Gilead, Sanofi, Spectrum, Amgen, Aptevo, BRIM bio, Acerta, I-Mab-pharma, Takeda, Compliment, Asana Bio, and Incyte: Honoraria; Seattle Genetics, Pfizer, Janssen, Gilead, Sanofi, Spectrum, Amgen, Aptevo, BRIM bio, Acerta, I-Mab-pharma, Takeda, Compliment, Asana Bio, and Incyte.: Consultancy; Teva, Bristol-Myers Squibb, Merck, Takeda, Seattle Genetics, Pfizer, Janssen, Takeda, and Effector: Research Funding.
Ibrutinib is not approved for previously treated transformed indolent B-cell lymphoma.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal