Background:
Acquired thrombotic thrombocytopenic purpura (aTTP) is a rare, life-threatening emergency caused by auto-antibodies against ADAMTS13. Current standard therapy utilizes plasma exchange (PLEX) and corticosteroids. Although this induces remission, disease relapse remains a common problem. Since more than 90% of aTTP is caused by an antibody to ADAMTS13, additional immunosuppressive therapy with rituximab (RTX) given upfront has been shown to lower relapse rates. An alternative therapy, Cyclophosphamide (CTX) has been used in relapsed disease, but data on its use in upfront management is limited to case reports only. Our study aims to compare outcomes at our institution between upfront CTX, RTX, and standard therapy alone. Our secondary objective is to identify initial presenting features that are predictive of higher relapse risk.
Methods:
In a retrospective cohort study, we identified all patients at our institution with a diagnosis code of TTP (ICD 9, 10: 446.6, M31.1) between 2009 and 2019. We only included patients with a confirmed diagnosis of aTTP, defined as having an ADAMTS13 level <10%, and either a positive ADAMTS13 inhibitor or antibody. We excluded patients with follow-up of less than 30 days, or thrombotic microangiopathy (TMA) due to other causes. Relapse was defined as recurrence of TMA in addition to an ADAMTS13 level <10%, or "laboratory relapse" evidenced as an acute drop of ADATMS13 level with a positive inhibitor with/without TMA. Time to first relapse was measured from the onset of remission, defined as the time of normalization of both platelets and lactate dehydrogenase (LDH) for at least 48 hours, until the time of relapse. The cumulative incidence of relapse (CIR) was estimated using Kaplan-Meier method, and its difference among treatment groups was examined by log-rank test. The effect of continuous and categorical covariates on relapse rate was estimated by univariate Cox model. The association of categorical variables was examined using chi-square test and the difference of continuous measurements among groups was tested using T-test or ANOVA.
Results:
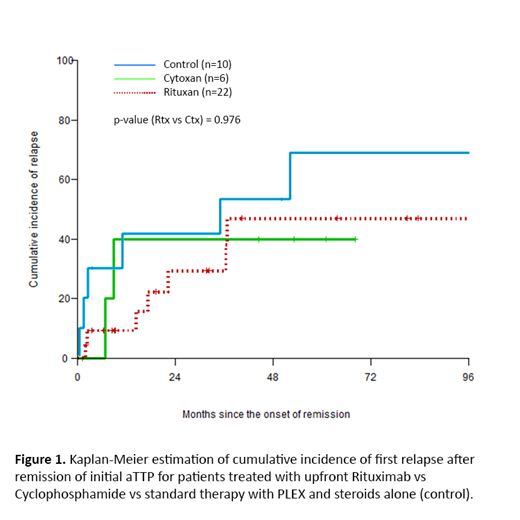
A total of 42 patients with a diagnosis of aTTP were identified in our cohort. The average age at diagnosis was 43.7 years. All patients received standard therapy with PLEX and steroids upon initial diagnosis. The prophylaxis group (n=29) received additional upfront therapy with either RTX (n=22) or CTX (n=6), and the control group (n=12) was treated with PLEX and steroids alone. There were no significant differences in the baseline characteristics between both groups. The median time to first relapse was 34.9 months in the control group, and 108.3 months in the prophylaxis group. Treatment with standard therapy alone was associated with a multi-variate hazard risk of 6.38 (95% CI: 1.1-37.7, p<0.05) for time to initial relapse. CIR at 2, 4, and 8 years was higher in the control group (41.7%, 53.3%, and 68.8%) as compared to the prophylaxis group (31.3%, 43.8%, and 43.8%, respectively). No difference was noted in CIR with CTX versus RTX, which was 40% at 4 years with CTX compared to 47% with RTX, p = 0.97 (Figure 1). Similarly, no statistically significant difference was noted in the time to first remission between CTX and RTX treatment (18 days in with CTX versus 14.9 days with RTX, p=0.583). Inhibitor titer at diagnosis correlated inversely with duration of remission (HR: 1.29, 95% CI: 1.03-1.61, p<0.05). Initial presenting platelet count, peak LDH value or co-existing autoimmune disease were not predictive of the duration of remission.
Conclusion:
Our study is the first to examine outcomes in a subset of patients treated with upfront CTX therapy for initial aTTP, and suggests similar time to first remission and 4-year CIR as compared to RTX. Our institutional experience suggests that CTX may be considered as an alternative therapy in patients intolerant to RTX. However, given the small group of patients treated with CTX, larger, prospective studies are warranted to confirm this observation. Consistent with currently published literature, PLEX and steroid therapy alone was associated with a significantly shorter duration of remission compared to additional immunosuppressive therapy. Furthermore, higher inhibitor titers were predictive of a shorter duration of remission, suggesting a role for aggressive upfront immunosuppressive treatment in these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal