Background
Immune-mediated thrombotic thrombocytopenic purpura (iTTP) is an autoimmune disorder caused by neutralizing anti-ADAMTS13 autoantibodies. This condition leads to life-threatening microvascular thrombi in systemic organs due to an imbalance between ADAMTS13 and von Willebrand factor. While several European groups reported that HLA-DRB1*11 was one of the strongest genetic risk factors for iTTP, no large-scale studies have analyzed which HLA alleles convey greater risk for iTTP in genetically isolated Japanese. Therefore, we analyzed ten HLA loci using next-generation sequencing.
Materials and Methods
We performed a prospective cohort study among Japanese patients with iTTP. The diagnosis of iTTP was suspected in cases of thrombocytopenia and hemolytic anemia with unknown cause, and was confirmed by both severe deficiency of ADAMTS13 (below 10% of normal) and the presence of anti-ADAMTS13 inhibitor. Fifty-six patients with iTTP from 19 institutes were enrolled in this study from August 2017 to March 2019, and 52 patients were finally eligible. An EDTA-treated serum sample was obtained from each patient at enrollment, and was analyzed via next-generation sequencing to identify the HLA alleles at following loci: A, B, C, DRB1, DRB3/4/5, DQA1, DQB1, and DPB1. Then, we compared allele frequencies at each locus in iTTP patients with those in a healthy Japanese population as reported by Nakajima et al in 2001. Additionally, we collected data on laboratory tests and clinical response to treatment during the acute phase. The HLA allele frequency of patients with iTTP and controls were compared by Fisher's exact test, and Bonferroni correction was applied to observed P-values. In this study, we multiplied the P-value by the number of alleles in each locus whose frequency was more than 1% in control to calculate the corrected P-value (Pc). This study was approved by the IRB of each referring institute.
Results
The male/female ratio of enrolled patients was 22/30. The median age was 58 years (range: 1-81). Based on the underlying disease, iTTP patients were classified as having primary TTP (n=38), autoimmune disease (n=12), malignancy (n=1), or acute pancreatitis (n=1). Plasma levels of ADAMTS13 activity were less than 3% in all cases, and the median concentration of ADAMTS13 autoantibodies was 2.5 Bethesda units/mL (range: 0.5-113). All patients showed severe thrombocytopenia (median platelet count: 12×109/L) and hemolytic anemia (median hemoglobin level: 8.0 g/dL, and median LDH level: 995 U/L). During the acute phase, 49 of 52 patients received combination treatment with plasma exchange (PEX) using fresh frozen plasma and corticosteroids. Additional immunosuppressants were administered in several cases, as follows: rituximab in 23 cases, cyclosporin A in 7 cases, cyclophosphamide in 5 cases, vincristine in 3 cases, and mycophenolate mofetil in 1 case. The median number of PEX treatments was 11 (range: 3-42).
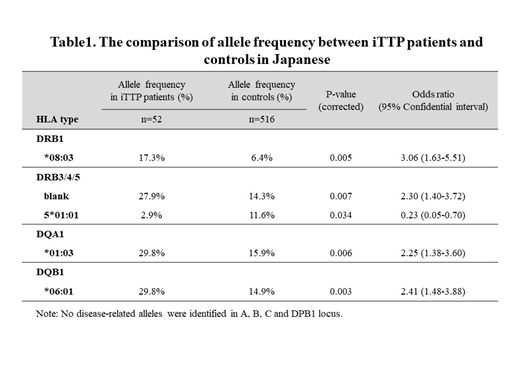
The allele frequencies in iTTP patients and controls are shown in Table 1. Regarding HLA class II alleles (DRB1, DRB3/4/5, DQA1, and DQB1), we identified the following alleles as risk factors for iTTP in the Japanese population: DRB1*08:03 (odds ratio [OR]: 3.06, Pc=0.005), DRB3/4/5*blank (OR: 2.3, Pc=0.007), DQA1*01:03 (OR: 2.25, Pc=0.006), and DQB1*06:01 (OR: 2.41, Pc=0.003). The estimated haplotype consisting of these 4 alleles was more frequent in the iTTP group than in the control group (30.8% vs. 6.0%, Pc<0.001). By contrast, DRB5*01:01 was associated with a reduced risk of iTTP (OR: 0.23, Pc=0.03). Among the A, B, C, and DPB1 loci, no significant difference was found between the 2 groups. Surprisingly, DRB1*11 was not identified as a risk factor for iTTP in Japanese, unlike in Caucasians. Additional analysis showed that this haplotype did not influence platelet count, hemoglobin level, lactate dehydrogenase level, ADAMTS13 activity, or the concentration of ADAMTS13 autoantibodies.
Conclusion
We found that a Japanese-specific haplotype, DRB1*08:03-DRB3/4/5(blank)- DQA1*01:03-DQB1*06:01, was a significant risk factor for iTTP in a Japanese population, and that DRB5*01:01 was a protective factor against iTTP development.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal