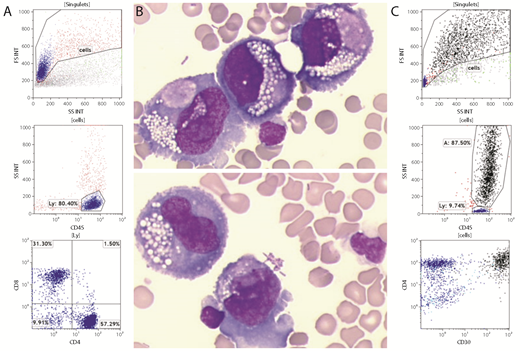
A 69-year-old woman who had a mastectomy with reconstruction using a textured implant 14 years ago presented with a periprosthetic effusion that was investigated for breast implant–associated anaplastic large-cell lymphoma (BIA-ALCL) by aspiration for cytology and flow cytometry (FCM). Although FCM analysis using the routine forward scatter/side scatter (FSC/SSC) settings primarily showed a population of normal T lymphocytes (panel A), cytology revealed atypical large pleomorphic cells with abundant vacuolated basophilic cytoplasm and prominent nucleoli (panel B, original magnification ×500; May-Grünwald-Giemsa stain). Thus, a second FCM analysis was performed with decreased FSC/SSC voltage and gain values. These modified settings detected CD45+/CD3−/CD4+/CD2+/CD5−/CD7− cells with high FSC/SSC and strong expression of CD30 (panel C). Immunohistochemistry performed on the capsulectomy specimen confirmed the diagnosis of BIA-ALCL.
Most BIA-ALCL patients have disease that is localized to the capsule with an excellent outcome after surgery alone. However, cases like the one presented here with tumor cells spreading to adjacent lymph nodes or other organs (bone metastases) have a worse prognosis and require chemotherapy in addition to capsulectomy. This case highlights the contribution of cytology and FCM to the diagnosis of BIA-ALCL; however, modified FSC/SSC settings are needed to avoid false-negative FCM results.
A 69-year-old woman who had a mastectomy with reconstruction using a textured implant 14 years ago presented with a periprosthetic effusion that was investigated for breast implant–associated anaplastic large-cell lymphoma (BIA-ALCL) by aspiration for cytology and flow cytometry (FCM). Although FCM analysis using the routine forward scatter/side scatter (FSC/SSC) settings primarily showed a population of normal T lymphocytes (panel A), cytology revealed atypical large pleomorphic cells with abundant vacuolated basophilic cytoplasm and prominent nucleoli (panel B, original magnification ×500; May-Grünwald-Giemsa stain). Thus, a second FCM analysis was performed with decreased FSC/SSC voltage and gain values. These modified settings detected CD45+/CD3−/CD4+/CD2+/CD5−/CD7− cells with high FSC/SSC and strong expression of CD30 (panel C). Immunohistochemistry performed on the capsulectomy specimen confirmed the diagnosis of BIA-ALCL.
Most BIA-ALCL patients have disease that is localized to the capsule with an excellent outcome after surgery alone. However, cases like the one presented here with tumor cells spreading to adjacent lymph nodes or other organs (bone metastases) have a worse prognosis and require chemotherapy in addition to capsulectomy. This case highlights the contribution of cytology and FCM to the diagnosis of BIA-ALCL; however, modified FSC/SSC settings are needed to avoid false-negative FCM results.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal