In this issue of Blood, Liu and colleagues demonstrate that gait speed is a valuable predictor of outcomes in older adults with hematologic malignancies, independent of age, performance status, comorbidities, aggressiveness of malignancy, and treatment type.1 Four hundred forty-eight adults with hematologic malignancies aged 75 years and older underwent geriatric screening at their initial consultation, including gait speed and grip strength testing, cognitive screening, and 2 frailty measures. The authors showed that gait speed predicted unplanned hospitalizations, emergency department visits, and survival, with each 0.1-m/s decrease in gait speed increasing mortality by 20%.
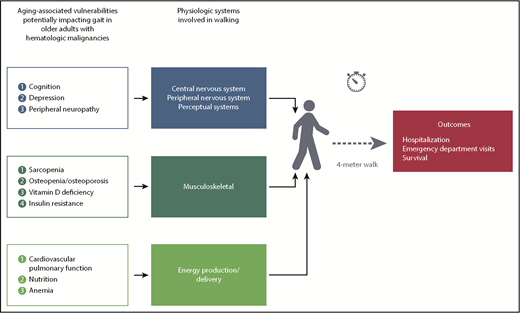
Slower gait speed results from convergence of aging-associated vulnerabilities on physiologic systems involved in walking.
Slower gait speed results from convergence of aging-associated vulnerabilities on physiologic systems involved in walking.
Numerous studies show that traditional oncology approaches, such as performance status, do not fully encompass the heterogeneous health statuses in older adults, and geriatric-focused approaches are needed. In response to the strong evidence of the value of applying geriatric principles to oncology patients, the American Society of Clinical Oncology issued guidelines for Geriatric Oncology last year.2 Abel and Klepin also recently reviewed the current body of literature for measuring frailty in older adults with hematologic malignancies.3 In the present study, gait speed was robustly predictive, and adding additional measures of frailty to the model did not substantially further improve predictive power.
How can such a simple test provide such robust risk prediction? Although measuring gait speed is simple, walking is quite complex, with multiple systems working in concert to effect locomotion (see figure). Six different physiologic systems contribute to ambulation: the central nervous system, the peripheral nervous system, the perceptual system, muscles, bones/joints, and energy production/delivery.4 Aging-associated vulnerabilities that are prevalent in older adults with hematologic malignancies (including cognitive impairment, depression, sarcopenia, cardiopulmonary comorbidities, and anemia, among others) converge to impact gait speed. This convergence likely underlies its robustness; when complementary deficits or single-system dysfunctions are sufficiently perturbing to impact gait speed, they are of predictive and prognostic significance.
The simplicity of gait speed makes it an attractive “frailty vital sign.” It takes <1 minute to complete and requires no special equipment to perform: at a minimum, the distance must be measured (4 meters in this study) and a timing device must be available (present on most smartphones). It need not be measured at every clinic visit; measurement at decision points or after a change in clinical status would be most instructive. Smartphone applications that calculate gait speeds from elapsed time measurements are available. In addition to GPS (Global Positioning System)-enabled patient badges available in some clinics, other emerging options for passive gait speed measurement include wearable devices, ultrasonic sensor devices, and floor sensor mats.5 Some clinic facilities incorporate means for assessing older adults in their design, installing floor tiles that act as distance markers for gait speed measurement.
A key advantage of gait speed is its safety for even quite frail patients; other measures, such as the Short Physical Performance Battery or the Timed Up and Go, have balance components that may be difficult or even dangerous for the most frail patients. As a measure, its floor effect (lowest level measurable) is only reached if the patient is nonambulatory, and it is not limited by a ceiling effect (highest level measurable) in the fittest patients. It discriminates among those with preserved Eastern Cooperative Oncology Group performance statuses of 0 to 1; its prognostic utility was as robust in the subgroup with a “good” performance status as the overall cohort. Its measurement as a continuous variable allows individualization of risk estimates, whereas well-established cutoffs from the general geriatrics literature inform what interventions should be triggered at certain gait speeds. For example, a gait speed <1.0 m/s (2.2 miles per hour) signifies increased risk of falls and warrants referral to physical therapy. Unlike other approaches to frailty, which are largely static over time, gait speed is highly responsive to change as a measure, which is particularly important in patients with hematologic malignancies, where clinical status can change rapidly.
In this study, additional measures of frailty did not substantially improve mortality prediction. This does not diminish the utility of other domains of geriatric assessment, such as instrumental activities of daily living, cognition, or polypharmacy. Gait speed serves as both a prognostic tool and a screening test to identify individuals who would benefit from additional intervention. There is clear utility to evaluating all of the cardinal domains of geriatric assessment. Several prior studies have demonstrated the independent prognostic significance of cognitive impairment in hematologic malignancies.6-8 In addition, vulnerabilities identified in geriatric assessment, such as fall risk, polypharmacy, and depression, warrant interventions, which directly improve patient outcomes.9
What work remains to refine the role of gait speed and other components of geriatric assessment in the management of older adults with hematologic malignancies? One might argue that external validation of the model is needed prior to measuring gait speed in hematology clinics. However, the evidence supporting the use of gait speed in older adults in general is already extremely strong,10 so its use is already valid. Additional evidence is needed to determine whether adjusting treatment recommendations based on gait speed or other aging-associated vulnerabilities will reduce toxicity, improve quality of life, or better help older adults meet their treatment goals. Another important step will be incorporating frailty into disease-focused staging systems, allowing integration of the aging-centered risk factors with disease-specific factors.
In summary, Liu et al have shown that a simple test requiring <1 minute to perform provides robust prognostic and predictive information in older adults with hematologic malignancies. Performance status alone is inadequate and should not be used as a sole measure of an older patient’s function. Although comprehensive assessment of multiple geriatric domains remains difficult within the constraints of most clinics, gait speed measurement is both an efficient and a valuable clinical measure for all older patients, when comparing the hazard ratio here to biomarkers of disease risk that are unquestionably obtained. Equal weight should be given to staging the aging as is for staging the malignancy in our older patients. I, for one, will be adding a tape measure and a stopwatch to my clinic essentials.
Conflict-of-interest disclosure: T.M.W. receives research funding from Janssen and is a consultant for Carevive Systems.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal