Abstract
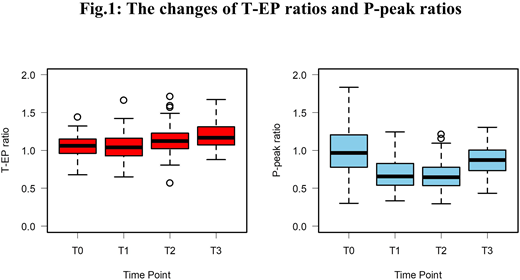
Introduction: L-asparaginase (L-Asp) is one of the risk factor of thromboembolism during ALL chemotherapy. Although the pathogenesis has been still unclarified, L-Asp may have profound effects on hepatic synthesis of pro-, anti-coagulant and fibrinolytic factors. In addition, recent studies demonstrated that the age of over 10-years might be a risk factor for this L-Asp associated coagulopathy. In this study, we hypothesized that change of balance between coagulation and fibrinolysis contributes to hyper-coagulation condition during chemotherapy including L-Asp. In order to clarify our hypothesis, we investigated the global coagulation and fibrinolytic function during the ALL induction therapy with simultaneous thrombin and plasmin generation assay (T/P-GA). Patients: Seventy-two pediatric patients aged 1.0 to 15.2 years (43 males and 29 females) with newly diagnosed ALL were enrolled from Aug. 2014 to Mar. 2018 at four hospitals in Japan. All patients and their families had no thrombotic predisposition. Fifty-five cases (76.4%) (BCP-ALL; n=47, T-ALL; n=7, MPAL; n=1) received BFM-95 oriented protocol consisting of a total of 8 doses of E.coli L-Asp 5,000 U/m2, whilst the others (BCP-ALL; n=13, T-ALL; n=2, MPAL; n=1, Ph-ALL; n=1) received Japan Association of childhood Leukemia Study (JACLS)-ALL02-protcol consisting of a total of 6 doses of E.coli L-Asp 6,000 U/m2. Fifty-two cases (72.2%) were categorized to younger group (1-10 years; median, 4.3 years) and the other cases to older group (>10 years; median, 12.6 years). The percentage of patients of each category were similar in the two treatment protocols (p=0.764). Methods: The global functions of coagulation and fibrinolysis were evaluated using T/P-GA [Matsumoto et al. TH 2013]. This clotting was initiated by the mixture of recombinant human tissue factor (Innovin®, f.c. 1 pM), phospholipid vesicles (f.c. 4 μM) and tissue-type plasminogen activator (f.c. 3.2 nM). Thrombin and plasmin generation were monitored simultaneously using thrombin- and plasmin-specific fluorogenic substrate (Z-Gly-Gly-Arg-AMC and BOC-Glu-Lys-Lys-MAC, respectively) in separate microtiter wells. The first derivatives (velocity) of thrombin and plasmin generation were utilized to derive the parameters, lag time (LT), endogenous potential (EP), peak levels (peak), and time to peak (ttPeak). EP of thrombin generation (T-EP) and plasmin-peak (P-peak) were selected as parameters for evaluation in this study. A ratio of T-EP and P-peak of patients' plasmas to those of control normal plasma were calculated. The conventional laboratory markers of coagulation and fibrinolysis were also monitored by fibrinogen (Fbg), fibrin-Fbg degradation products (FDP), antithrombin (AT), thrombin-AT complex and plasmin-α2 plasmin inhibitor complex. Plasmas were collected at T0; pre-phase of L-Asp, T1; intermittent phase of L-Asp, T2; post-phase of L-Asp, and T3; post induction phase. Results: None of the cases developed L-Asp associated coagulopathy, and two cases (2.8%) developed induction failure. Thirteen cases (18.1%) received fresh frozen plasma transfusion for low Fbg level, whilst 52 (72.2%) cases received AT supplement for low AT level. Fbg showed a median of 165, 99.0, 97.0 and 316 mg/dl at T0, T1, T2 and T3, respectively, and AT showed a median of 143, 80.9, 80.0 and 105%, respectively, whilst the value of other conventional markers remained within reference value. T-EP revealed a median of 1,134, 1,135, 1,221, 1,277 and 1,102 nM, whilst P-peak showed a median of 5.33, 3.75, 3.63, 4.91 and 5.51 nM for T0, T1, T2, T3 and control plasma, respectively, indicating the elevated T-EP ratios and reduced P-peak ratios (Fig. 1). T-EP ratios showed significantly higher at T2 and T3 than at T0 and T1 (p<0.05), whilst P-peak ratios showed significantly lower at T1 and T2 than at T0 and T3 (p<0.01) (median ratios of T-EP/P-peak; T0; 1.06/0.97, T1; 1.04/0.65, T2; 1.12/0.65, T3; 1.17/0.87, respectively). P-peak ratios of the older group showed significantly lower than the younger group at T1 (median; 0.58 vs 0.69, p=0.016). Conclusion: The results from T/P-GA showed that their hemostatic dynamics appear likely to shift to hyper-coagulation and hypo-fibrinolysis at L-Asp treatment phase. These results suggest that the imbalance of coagulation and fibrinolysis might cause thrombotic complication during the L-Asp treatment for ALL, especially in patients aged 10-years older.
Nogami:Chugai Pharmaceutical Co., Ltd: Consultancy, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties: Anti-FIXa/X bispecific antibodies , Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal