Abstract
BACKGROUND: Increasing numbers of women with sickle cell disease (SCD) are reaching reproductive age. There is an array of possible pregnancy outcomes that women with SCD may experience. Many have described adverse maternal and fetal outcomes in pregnant patients with SCD including increased risk of pre-eclampsia, infections, painful vaso-occlusive crises as well as increased risk of intrauterine growth restriction, pre-term delivery and pregnancy loss. Not all women with SCD have complicated pregnancies, however. Limited data are available to categorize the proportion of patients who have uncomplicated pregnancies and protective characteristics for good pregnancy outcomes. Identifying these features potentially informs practice and reduces exposure to blood products as red blood cell (RBC) transfusion is associated with an increased risk of alloimmunization, particularly in pregnancy.
OBJECTIVE: To determine the proportion and characteristics of pregnant patients with SCD who have uncomplicated pregnancies.
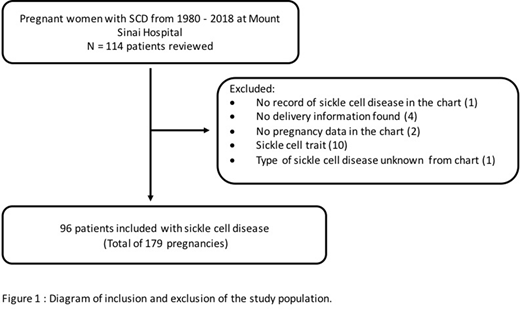
METHODS: We retrospectively reviewed medical records of pregnant women with SCD from 1980 to 2018 at Mount Sinai Hospital, a university affiliated tertiary care centre in Toronto, Canada. We defined a pregnancy to be uncomplicated if the pregnancy was not associated with a hospitalization, RBC transfusion was not administered peripartum and/or the delivery was at term (37 or more weeks gestation).
RESULTS: A total of 179 pregnancies were included (Figure 1). Preliminary results show that 57% of pregnancies had hemoglobin SS disease. The median maternal age was 27 years (range 16-43 years) (n=179). Median hemoglobin concentration, platelet count and leukocyte count were 91g/L (n=141), 304 x 10(9)/L (n=140) and 11 x 10(9)/L (n=140), respectively. Hospital admission was required in 61% of pregnancies (n=171) and RBC transfusion in 49% of pregnancies (n=173). The median hemoglobin F level was 0.05 (range 0.01-0.87). Nineteen percent had coexisting alpha gene deletion (s). The median birth weight was 2863 grams (n=155). Analysis is ongoing to determine characteristics associated with the pre-defined pregnancy outcomes.
CONCLUSIONS: Women with SCD frequently have adverse maternal and fetal outcomes with pregnancy. However, 39% of pregnancies with SCD in this study did not require hospitalization and 51% did not require RBC transfusion. Additional analysis will attempt to identify protective features so as not to expose all patients to RBC transfusion unless it is required. These initial results suggest that risk scores should be developed for pregnant patients with sickle cell disease to identify who may benefit from RBC transfusion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal