Abstract
Background: Bronchiolitis obliterans syndrome (BOS), chronic graft versus host (cGVHD) disease of the lungs after hematopoietic cell transplantation, is characterized by fixed airway obstruction, bronchiolar inflammation, and scarring and confers a dismal prognosis. While steroids are the backbone therapy for BOS, prolonged use is not recommended. There is no consensus therapy for patients who are steroid dependent or refractory (SR). Ruxolitinib, a JAK1/2 inhibitor, has potent anti-inflammatory effects by modifying T and dendritic cell signaling. It is FDA approved to treat acute GVHD, though there are also reports of its efficacy in cGVHD. We describe the experience of children with SR BOS treated with ruxolitinib.
Methods: IRB approval was obtained for retrospective review of all patients treated with ruxolitinib for SR BOS after allogenic HCT. Patients were identified using departmental records. BOS was defined as SR if patients had worsening pulmonary function tests (PFTs) on therapy or required ≥0.5 mg/kg/day of steroids for greater than 30 days. 2014 NIH consensus conference criteria were used to define PFT diagnostic criteria for BOS and response to therapy. A partial response (PR) was an improvement in FEV1 of 10% and complete response (CR) an FEV1 of ≥80% predicted.
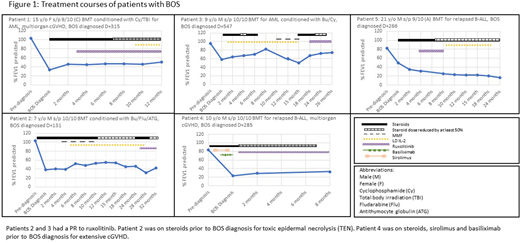
Results: Five patients were treated with ruxolitinib for SR BO; 2 patients had no response to steroids and 3 were unable to wean (Figure 1). All patients received an unrelated bone marrow transplant (BMT) and the same aGVHD prophylaxis; methotrexate on days + 1, 3, 6, and 11, cyclosporine, and steroids. 3/6 patients were matched at 10/10 HLA-loci and 2 at 9/10. One patient (#5) received a second BMT for relapsed MDS, all other patients had one BMT. 2/5 patients had acute GVHD that was steroid responsive and resolved prior to BOS diagnosis.
BOS developed a median of 285 days after stem cell infusion (range 131-547 days). 4/5 patients presented with dyspnea, and 1 (#4) developed a new oxygen requirement. He was developmentally delayed and could not report symptoms. Patient 4 developed extensive cGVHD 11 months after receiving a donor lymphocyte infusion for relapse of AML 3 months after HCT. Patients 2 and 5 had a concurrent pulmonary fungal infection at the time of diagnosis. Median FEV1% of predicted at diagnosis was 38% (range 23-64%). All patients were treated with corticosteroids and fluticasone, montelukast, azithromycin (FAM) after diagnosis of BOS. Ruxolitinib ranged from the third to fifth line therapy. 2/5 patients had a PR to ruxolitinib with an increase in predicted FEV1% of 10 and 24% (#2 and 3 respectively). One patient (#4) had an increase of FEV1 of 9% and was able to stop steroids. Patient 1 had stable PFTs and was able to wean steroids by 83%. Median time to response was 4 weeks.
Patient 5 was treated for 4 months with ruxolitinib and was not able to have any pulmonary function tests (PFTS) during this period because of a pneumothorax. When this resolved, he had new nodules on chest CT, worsened PFTs and was found to have culture confirmed pulmonary Nocaria and Hypodontia palmae. Ruxolitinib was discontinued in the setting of a new infection. Without interim PFTs, his response was considered non-evaluable. He continues to have progressive BOS on corticosteroids and had a third relapse of his MDS. Other than this infection, the other 4/5 patients had no side effects from ruxolitinib. Doses ranged from 2.5 mg three times a week in a patient with end stage renal disease to 10 mg BID. 3/6 patients had extensive cGVHD with multiple organs involved; all other organ systems had a PR or CR to ruxolitinib. All patients are alive and 4/5 are disease free. Median follow up period after BOS diagnosis was 2 years (range 8-32 months).
Conclusion: We describe 5 pediatric patients with SR BOS after hematopoietic cell transplantation. In the 4 patients with an evaluable response, 50% (2/4) had a PR to ruxolitinib and an additional patient had an improvement in predicted FEV1 of 9%. All were able to stop steroids or wean the dose by at least 50%. Responses occurred early, and the medication was well tolerated with minimal side effects. This is a small case series, but describes both improvement in pulmonary function testing and the ability to wean steroids after treatment with ruxolitinib in children with SR BOS - two measures notoriously difficult to obtain. Further prospective studies are needed to evaluate the role of ruxolitinib in children with cGVHD, particularly BOS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal