Abstract

Background: Haploidentical (Haplo) hematopoietic cell transplantation (HCT) provides an alternative option for patients without HLA-matched donor. GVHD, engraftment failure, and infectious complications continue to be the main causes of non-relapse mortality (NRM). We hypothesized that selective depletion of TCRαβ+ and CD45RA+ naïve T cells subset will permit hematopoietic engraftment, while effectively reducing GVHD, and provide improved donor immune reconstitution through adoptive transfer of donor's mature NK and γδ T cells and CD45RA- memory T cells.
Methods: GCSF +/- plarixefor (N=13) mobilized PBSC apheresis product were divided into two fractions in 9:1 ratio, and depleted using CliniMACS device after labeling with TCRαβ and CD45RA reagents (Miltenyi Biotec, Bergish-Gladbach, Germany), respectively. The conditioning regimen consisted of total nodal irradiation 6 - 7.5 Gy over 3 equal fractions, 160 mg/m2 Fludarabine divided daily over 4 days, Thiotepa 10 mg/kg divided twice daily for 1 day and Melphalan 70-140 mg/m2 for 1 day. Short term GVHD prophylaxis for 30 days was given to 1 patient using MMF, 11 using tacrolimus or 2 using Sirolimus.
Results: We transplanted 20 adults (median age 42 years, range 20 - 68 ) and 3 children (age range 7-14 years) with high risk AML (n=14), ALL (n=6), MDS (n=2), myeloma (N=1). The patients were infused with TCRαβ and CD45RA depleted graft containing a median of 9.94 x 106 (range, 5.58 - 20.78) CD34+ cells/kg, 0.19 x 104 (range 0 - 8.53) CD45RA+CD3+ cells/kg, and 4.21 x 106 (range, 0.15 - 11.67) CD45RO+CD3+ cells/kg. In addition, the TCRαβ depleted graft fraction contained a median of 0.19 x 104 (range 0 - 8.53) TCRαβ+ cells/kg, and 8.87 x 106 (range 1.73 - 29.74) TCRγδ + cells/kg. All patients except 1 had engraftment of ANC > 500 cells/µL at a median of 11 day (range, 8 - 19) and PLT > 20,000 cells/µL at a median of 12 day (range, 7 - 19). Complete donor chimerism was seen at the time of engraftment in all patients with primary engraftment. Only 1 patient experienced primary graft failure. There was no secondary graft failure.
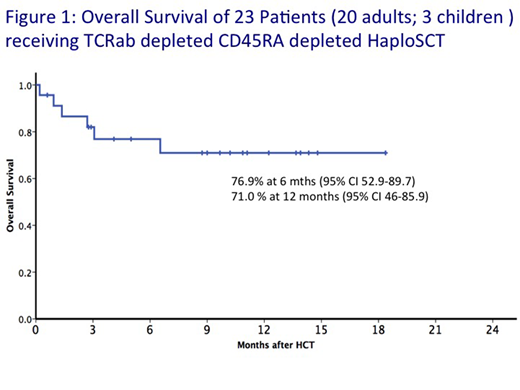
Eleven patients developed acute GVHD of grade II-IV, with the day 100 cumulative incidence (C.I.) of acute GVHD of Gd II-IV, and Gd III-IV of 50% (95% CI 27.3 - 69.0%) and 17.9 % (95% CI 5.3- 36.4%), respectively. One patient experienced chronic GVHD. Day 180 C.I. of NRM and relapse were 23.9 % (95% 8.3-43.9%) and 5.6 % (95% CI 0.3-23.3%), respectively. NRM was attributed to aGVHD in 3 of the 6 deaths. Viral reactivation included CMV (n=7), HHV6 (N=4), EBV (N=3) and adenovirus (N=2), with no fatal viral infection occurred within 100 days. Two patients had fatal blood stream infection within 100 days. With a median follow up of 306 days (range 18 - 551 days) in surviving patients, the 6 month and 1 year overall survival (OS) were 76.9% (95% CI 52.9-89.7%) and 71 % (95% CI 46-85.9%), respectively. (Figure 1).
Conclusions: Our preliminary results suggest that RIC haplo-HCT with TCRαβ and CD45RA+ depleted grafts allows successful allograft in high-risk patients lacking a suitable matched donor. NRM due to GVHD remains the major obstacle for the successful HCT. Fine adjustment of T cell dose with short course of immunosuppressant may reduce GVHD while preserving antitumor and antimicrobial immunocompetence.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal