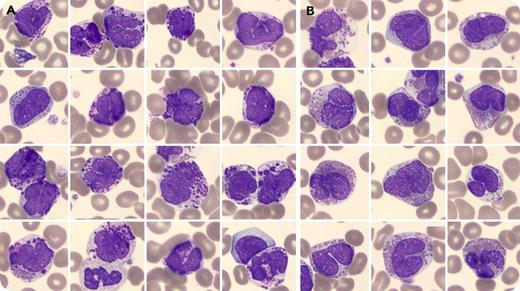
A 35-year-old man with a history of ankylosing spondylitis for which he received adalimumab was referred to our clinic because of marked leukocytosis detected from a routine blood test. He experienced occasional night sweats. He was found to have splenomegaly. The complete blood count showed normocytic anemia (13.37 g/dL, 90 fL), normal platelets (315 × 109/L), and leukocytosis (32.8 × 109/L) with basophilia (51%), eosinophilia (20%), promyelocytes (1%), and blasts (1%). Peripheral blood smear revealed prominent basophilia and atypical eosinophilia (panel A, atypical basophilic granulocytes; panel B, atypical eosinophilic granulocytes, with clearly visible cytoplasm, prominent nuclei, and an increased nuclear-cytoplasmic ratio; original magnification ×100, May-Grünwald Giemsa stain). Immunophenotyping showed a cell population negative for CD117, CD2, and CD25. Bone marrow biopsy showed increased cellularity with <10% myeloblasts as well as marked reticulin fibrosis. BCR-ABL1 fusion was negative. Conventional cytogenetics with gene-specific probes showed an extremely rare t(9;12)(q34;p13) resulting in the ETV6-ABL1 fusion. No additional cytogenetic abnormalities were observed, including no PDGFRa rearrangements.
The ETV6-ABL1 fusion induces a chronic myeloid leukemia–like disease with a more aggressive behavior and prominent basophilia. The patient received dasatinib with complete molecular response followed by an allogeneic transplantation.
A 35-year-old man with a history of ankylosing spondylitis for which he received adalimumab was referred to our clinic because of marked leukocytosis detected from a routine blood test. He experienced occasional night sweats. He was found to have splenomegaly. The complete blood count showed normocytic anemia (13.37 g/dL, 90 fL), normal platelets (315 × 109/L), and leukocytosis (32.8 × 109/L) with basophilia (51%), eosinophilia (20%), promyelocytes (1%), and blasts (1%). Peripheral blood smear revealed prominent basophilia and atypical eosinophilia (panel A, atypical basophilic granulocytes; panel B, atypical eosinophilic granulocytes, with clearly visible cytoplasm, prominent nuclei, and an increased nuclear-cytoplasmic ratio; original magnification ×100, May-Grünwald Giemsa stain). Immunophenotyping showed a cell population negative for CD117, CD2, and CD25. Bone marrow biopsy showed increased cellularity with <10% myeloblasts as well as marked reticulin fibrosis. BCR-ABL1 fusion was negative. Conventional cytogenetics with gene-specific probes showed an extremely rare t(9;12)(q34;p13) resulting in the ETV6-ABL1 fusion. No additional cytogenetic abnormalities were observed, including no PDGFRa rearrangements.
The ETV6-ABL1 fusion induces a chronic myeloid leukemia–like disease with a more aggressive behavior and prominent basophilia. The patient received dasatinib with complete molecular response followed by an allogeneic transplantation.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal