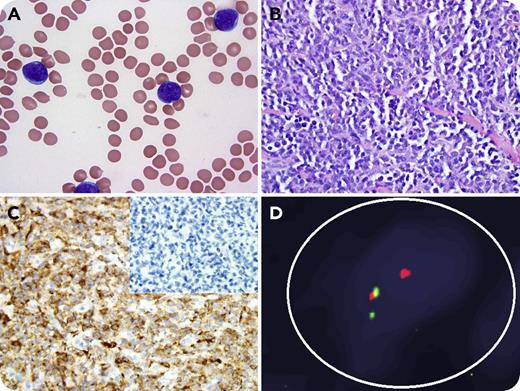
A 77-year-old man was diagnosed with B-cell acute lymphoblastic leukemia (ALL). Peripheral blood (panel A; original magnification ×100, Wright-Giemsa stain) showed medium-sized lymphoblasts with fine chromatin and multiple small nucleoli. By flow cytometry, the blasts expressed CD15, CD19, CD22, CD33 (dim, subset), CD38, CD45 (dim), PAX5, HLA-DR, and Tdt (dim). Cytogenetic analysis showed 46,XY,t(4;11)(q21;q23) consistent with a KMT2A(MLL)-AFF1(AF4) translocation. The patient was treated on the frontline blinatumomab study (NCT02143414) and achieved complete remission (CR) with negative minimal residual disease by multicolor flow cytometry. Eight months later, he presented with a subcutaneous mass on his chest, and biopsy showed sheets of medium-to-large atypical cells with fine chromatin and small nucleoli, consistent with myeloid sarcoma (panel B; original magnification ×20, hematoxylin and eosin stain). Immunohistochemical stains of tumor cells were positive for CD33, CD43, and lysozyme (panel C; original magnification ×20) but negative for CD19, PAX5 (panel C, inset), and Tdt. Fluorescence in situ hybridization for MLL (green signal, 5′ end; red signal, 3′ end) from the mass was positive for rearrangement (panel D). The bone marrow was negative for involvement by acute leukemia. The patient was treated with azacitidine and venetoclax and achieved CR.
Extramedullary escape and CD19 antigen loss are patterns of relapse following blinatumomab (CD3/CD19-bispecific T-cell engager) therapy in ALL. Interestingly, MLL+ ALL has the ability to undergo a myeloid lineage switch under the pressure of ALL-targeted therapies as a mechanism of resistance and adaptation.
A 77-year-old man was diagnosed with B-cell acute lymphoblastic leukemia (ALL). Peripheral blood (panel A; original magnification ×100, Wright-Giemsa stain) showed medium-sized lymphoblasts with fine chromatin and multiple small nucleoli. By flow cytometry, the blasts expressed CD15, CD19, CD22, CD33 (dim, subset), CD38, CD45 (dim), PAX5, HLA-DR, and Tdt (dim). Cytogenetic analysis showed 46,XY,t(4;11)(q21;q23) consistent with a KMT2A(MLL)-AFF1(AF4) translocation. The patient was treated on the frontline blinatumomab study (NCT02143414) and achieved complete remission (CR) with negative minimal residual disease by multicolor flow cytometry. Eight months later, he presented with a subcutaneous mass on his chest, and biopsy showed sheets of medium-to-large atypical cells with fine chromatin and small nucleoli, consistent with myeloid sarcoma (panel B; original magnification ×20, hematoxylin and eosin stain). Immunohistochemical stains of tumor cells were positive for CD33, CD43, and lysozyme (panel C; original magnification ×20) but negative for CD19, PAX5 (panel C, inset), and Tdt. Fluorescence in situ hybridization for MLL (green signal, 5′ end; red signal, 3′ end) from the mass was positive for rearrangement (panel D). The bone marrow was negative for involvement by acute leukemia. The patient was treated with azacitidine and venetoclax and achieved CR.
Extramedullary escape and CD19 antigen loss are patterns of relapse following blinatumomab (CD3/CD19-bispecific T-cell engager) therapy in ALL. Interestingly, MLL+ ALL has the ability to undergo a myeloid lineage switch under the pressure of ALL-targeted therapies as a mechanism of resistance and adaptation.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal