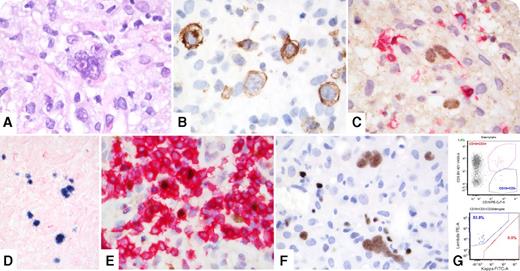
A 66-year-old man was diagnosed with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) in 2006, observed until 2011, and then treated with fludarabine/cyclophosphamide/rituximab followed by ibrutinib/venetoclax without complete remission. In 2017, an abdominal computed tomography scan showed increasing hepatosplenomegaly and multicompartmental lymphadenopathy. A right axillary lymph node biopsy showed a lymphohistiocytic infiltrate containing Hodgkin-Reed-Sternberg cells (panel A; original magnification ×1000 with oil immersion, hematoxylin and eosin stain), positive for CD15 (subset), CD30 (strong) (panel B; original magnification ×1000 with oil immersion, CD30 immunohistochemical stain), PAX-5 (weak) (panel C; original magnification ×1000 with oil immersion, PAX5/CD5 dual immunohistochemical stain), and Epstein-Barr virus (EBV)–encoded RNA (panel D; original magnification ×400, in situ hybridization stain). Dual-staining with anti-CD5 and anti-PAX-5 antibodies showed residual CLL/SLL cells with aberrant coexpression of CD5 and PAX-5 (panel E; original magnification ×1000 with oil immersion, PAX5/CD5 dual immunohistochemical stain). Both cell types were positive for LEF-1 (panel F; original magnification ×1000 with oil immersion, LEF-1 immunohistochemical stain). The bone marrow biopsy showed similar infiltrates (20% to 30% of cellularity). Flow cytometry showed a minute CD5 positive, λ restricted B-cell population in both specimens (panel G).
Progression to a more aggressive neoplasm, typically diffuse large B-cell lymphoma, occurs in approximately 5% of patients with CLL/SLL; however, about 0.4% of patients develop classical Hodgkin lymphoma. Treatment with fludarabine impairs immunosurveillance via T-cell toxicity, increasing susceptibility to EBV reactivation, and may promote progression. Because the clonal relationship between CLL/SLL and second neoplasm remains unclear, many authors advocate the term Richter “syndrome” instead of “transformation.” The LEF-1 staining of our case supports true transformation.
A 66-year-old man was diagnosed with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) in 2006, observed until 2011, and then treated with fludarabine/cyclophosphamide/rituximab followed by ibrutinib/venetoclax without complete remission. In 2017, an abdominal computed tomography scan showed increasing hepatosplenomegaly and multicompartmental lymphadenopathy. A right axillary lymph node biopsy showed a lymphohistiocytic infiltrate containing Hodgkin-Reed-Sternberg cells (panel A; original magnification ×1000 with oil immersion, hematoxylin and eosin stain), positive for CD15 (subset), CD30 (strong) (panel B; original magnification ×1000 with oil immersion, CD30 immunohistochemical stain), PAX-5 (weak) (panel C; original magnification ×1000 with oil immersion, PAX5/CD5 dual immunohistochemical stain), and Epstein-Barr virus (EBV)–encoded RNA (panel D; original magnification ×400, in situ hybridization stain). Dual-staining with anti-CD5 and anti-PAX-5 antibodies showed residual CLL/SLL cells with aberrant coexpression of CD5 and PAX-5 (panel E; original magnification ×1000 with oil immersion, PAX5/CD5 dual immunohistochemical stain). Both cell types were positive for LEF-1 (panel F; original magnification ×1000 with oil immersion, LEF-1 immunohistochemical stain). The bone marrow biopsy showed similar infiltrates (20% to 30% of cellularity). Flow cytometry showed a minute CD5 positive, λ restricted B-cell population in both specimens (panel G).
Progression to a more aggressive neoplasm, typically diffuse large B-cell lymphoma, occurs in approximately 5% of patients with CLL/SLL; however, about 0.4% of patients develop classical Hodgkin lymphoma. Treatment with fludarabine impairs immunosurveillance via T-cell toxicity, increasing susceptibility to EBV reactivation, and may promote progression. Because the clonal relationship between CLL/SLL and second neoplasm remains unclear, many authors advocate the term Richter “syndrome” instead of “transformation.” The LEF-1 staining of our case supports true transformation.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal