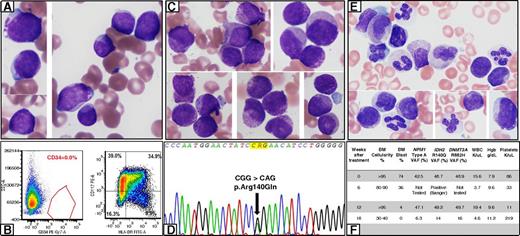
A 75-year-old woman was diagnosed with acute myeloid leukemia (AML). Bone marrow (BM) showed intermediate-sized blasts (78%) with scant agranular cytoplasm (panel A: Wright-Giemsa stain, original magnification ×1000) and occasional “fish-mouth” morphology. Auer rods were absent. Flow cytometry (FC) confirmed CD34-negative myeloblasts with CD117 and HLA-DR expression (panel B). Karyotype was diploid; next-generation sequencing (NGS) showed NPM1, IDH2, and DNMT3A mutations. She was treated on a clinical trial with azacitidine and an IDH2 inhibitor. Repeat BM (6 weeks) showed persistent AML. The blasts showed prominent cytoplasmic granulation: coarse primary (azurophilic) and fine secondary granules (panel C: Wright-Giemsa stain, original magnification ×1000). FC and IDH2 mutation analysis confirmed persistent disease (panel D, arrow). BM (12 weeks) showed 4% blasts. Many cells were difficult to characterize due to prominent cytoplasmic granulation (panel E: Wright-Giemsa stain, original magnification ×1000). FC was negative for residual disease; however, NGS showed all 3 mutations at a high allelic burden. BM (18 weeks) was negative by morphology and FC; NGS showed persistence of all 3 mutations (panel F: Hgb, hemoglobin; FITC-A, fluorescein isothiocyanate-A; PE-Cy7, phycoerythrin-cyanine 7; SSC-A, side scatter area; VAF, variant allele frequency; WBC, white blood cell).
The case illustrates the unique morphologic challenges encountered in this era of novel targeted therapies. IDH2 inhibitors induce differentiation of the blasts, manifested here as prominent cytoplasmic granulation. It is important to be aware of these morphologic alterations associated with IDH2 inhibitors and use a multimodal approach for residual disease detection.
A 75-year-old woman was diagnosed with acute myeloid leukemia (AML). Bone marrow (BM) showed intermediate-sized blasts (78%) with scant agranular cytoplasm (panel A: Wright-Giemsa stain, original magnification ×1000) and occasional “fish-mouth” morphology. Auer rods were absent. Flow cytometry (FC) confirmed CD34-negative myeloblasts with CD117 and HLA-DR expression (panel B). Karyotype was diploid; next-generation sequencing (NGS) showed NPM1, IDH2, and DNMT3A mutations. She was treated on a clinical trial with azacitidine and an IDH2 inhibitor. Repeat BM (6 weeks) showed persistent AML. The blasts showed prominent cytoplasmic granulation: coarse primary (azurophilic) and fine secondary granules (panel C: Wright-Giemsa stain, original magnification ×1000). FC and IDH2 mutation analysis confirmed persistent disease (panel D, arrow). BM (12 weeks) showed 4% blasts. Many cells were difficult to characterize due to prominent cytoplasmic granulation (panel E: Wright-Giemsa stain, original magnification ×1000). FC was negative for residual disease; however, NGS showed all 3 mutations at a high allelic burden. BM (18 weeks) was negative by morphology and FC; NGS showed persistence of all 3 mutations (panel F: Hgb, hemoglobin; FITC-A, fluorescein isothiocyanate-A; PE-Cy7, phycoerythrin-cyanine 7; SSC-A, side scatter area; VAF, variant allele frequency; WBC, white blood cell).
The case illustrates the unique morphologic challenges encountered in this era of novel targeted therapies. IDH2 inhibitors induce differentiation of the blasts, manifested here as prominent cytoplasmic granulation. It is important to be aware of these morphologic alterations associated with IDH2 inhibitors and use a multimodal approach for residual disease detection.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal