In this issue of Blood, Gramaglia et al1 have provided valuable data on whether platelets are protective in malaria infection by directly killing Plasmodium parasites, or deleterious by driving adverse immune responses. Platelets are the cellular mediators of thrombosis. Although this is a very important biologic role, platelets are also the most numerous circulating cell with an inflammatory and immune modulatory function. The first, and still the best understood, disease context for platelet-driven inflammation is atherosclerosis. More recently, platelets have been shown to have important, largely adverse roles, in infectious disease processes such as sepsis, bacterial infections, viral infections, and parasitic infections, including infections with the malaria causative agent Plasmodium. With an increased appreciation for the immune and inflammatory functions of platelets in many diseases, there have been an increased number of studies, including study into platelets in malaria infection. There have been conflicting conclusions on whether platelets are “good or bad” players in malaria infection. Although there is a broad sense that platelets are proinflammatory and initiate or accelerate immune cell responses to infection in general, some reports have indicated a potential direct anti-Plasmodium parasite-killing role for platelets (see figure). This paper by Gramaglia et al provides a further understanding of whether platelets directly kill Plasmodium parasites, and if they do, does it actually limit the in vivo parasite burden.
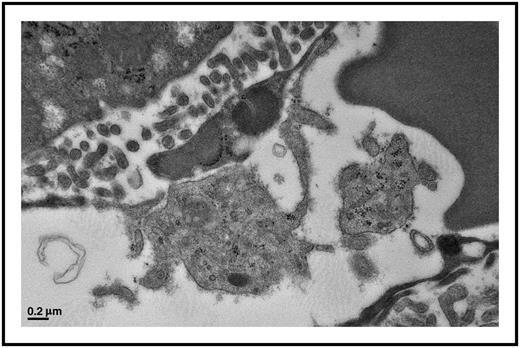
Platelets actively interact with liver endothelial cells in a Plasmodium berghei infection model. This platelet has formed a distinct contact interaction with the endothelial cell. These interactions occur in many tissue beds and with circulating immune cells contributing to the inflammatory pathogenesis of cerebral malaria. Electron microscopy image; scale bar, 0.2 μm.
Platelets actively interact with liver endothelial cells in a Plasmodium berghei infection model. This platelet has formed a distinct contact interaction with the endothelial cell. These interactions occur in many tissue beds and with circulating immune cells contributing to the inflammatory pathogenesis of cerebral malaria. Electron microscopy image; scale bar, 0.2 μm.
The work of numerous laboratories has shown that platelets are key mediators of both immune responses and immune development. Platelets contain a large and diverse array of granule-stored chemokines and cytokines, and when stimulated, platelets also de novo produce inflammatory molecules that promote leukocyte activation and trafficking, as well as vascular inflammation. Although small in size (∼2 µm in diameter), platelets have major immune effects due to their circulating numbers (∼200 000/µL in humans) and the numerous inflammatory molecules they contain. Malaria-infected red blood cells (RBCs) can activate platelets that increase cerebral vasculature endothelial inflammation, leukocyte recruitment, and loss of the blood-brain barrier. Immune and endothelial cell responses to infection also induce vascular inflammation, more local platelet activation, and platelet interactions with an intact and inflamed endothelial cell layer, further driving platelet adhesion, activation, and an amplification of vascular inflammation. Direct antibacterial properties have been described for platelets, including bacteria engulfment and clearance and the release of microbicidal proteins from platelets,2 leading to speculation that, similar to other immune cells, platelet immune responses may be protective and beneficial by directly clearing and killing pathogens.
So why the confusion on whether platelets are protective or deleterious in Plasmodium infection? Many studies have shown that in experimental cerebral malaria (eCM) platelets play a central role in the cerebral vascular disease pathogenesis,3,4 and thus, platelets are potentially “bad” in cerebral malaria. This concept is supported by human autopsy specimens.5 However, a few recent studies concluded that platelets may have a direct role in killing Plasmodium parasites in infected RBCs.6,7 This current study in Blood took a rigorous in vivo approach to show that although platelets drive an immune response to infection, they are unlikely to have direct protective in vivo parasite-killing functions.
There are many potential reasons for the different interpretations, including in vivo vs in vitro study, data analysis approaches, and interpretations, as well as the types of parasites used. Another very important factor is that we continue to better understand how platelets shape the immune response, and therefore, continue to gain a better understanding of how to best interpret in vivo platelet-related data. For example, the initial paper describing a potential direct parasite-killing role for platelets in malaria used an uncomplicated malaria (UM) model6 in which the immune response to infection is very different than eCM immune responses. eCM models have significant platelet activation. UM models develop thrombocytopenia with less evidence of platelet activation. Immune and vascular responses to eCM infection are more important than the parasite itself in driving platelet activation. In addition, studies using mice that are genetically platelet-deficient must be carefully interpreted. We have recently described major immune alterations in platelet-deficient mice, including increased numbers of T-helper 17 type of T cells, and that the platelet chemokine PF4 regulates T-helper responses.8 Therefore, interpretation of data from chronically platelet-deficient mice, particularly in more slowly developing infectious disease models like UM, must be carefully interpreted. The use of acute platelet depletion may be more appropriate in many situations, but again is complicated by the method used, such as introduction of a platelet-depletion antibody. This current study is very valuable in its thoughtful approach to measuring parasite burdens in acutely platelet-depleted and reconstituted mice. In addition, although models of eCM and UM are valuable in better understanding Plasmodium-related disease pathogenesis, separating the interpretation of each model and considering each independently are likely important distinctions due to their poorly understood differences in immune and vascular cell responses.
Any immune response is a double-edged sword: some are good for isolating, limiting, and clearing an infection, but exaggerated or prolonged immune responses can lead to tissue injury and long-term organ dysfunction. Understanding how platelets are active participants in well-validated model systems is therefore important to progress to a general understanding of vascular inflammatory disease pathogenesis.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal