Key Points
First prospective, controlled study to identify complex karyotypes as an independent prognostic factor of survival in CLL.
First study to show that mutations in KRAS or POT1 impact treatment response and survival after chemoimmunotherapy.
Abstract
Genetic instability is a feature of chronic lymphocytic leukemia (CLL) with adverse prognosis. We hypothesized that chromosomal translocations or complex karyotypes and distinct somatic mutations may impact outcome after first-line chemoimmunotherapy of CLL patients. We performed metaphase karyotyping and next-generation sequencing (NGS) of 85 genes in pretreatment blood samples obtained from 161 patients registered for CLL11, a 3-arm phase 3 trial comparing frontline chlorambucil (Clb) vs Clb plus rituximab (Clb-R) or Clb plus obinutuzumab in CLL patients with significant comorbidity. Chromosomal aberrations as assessed by karyotyping were observed in 68.8% of 154 patients, 31.2% carried translocations, and 19.5% showed complex karyotypes. NGS revealed 198 missense/nonsense mutations and 76 small indels in 76.4% of patients. The most frequently mutated genes were NOTCH1, SF3B1, ATM, TP53, BIRC3, POT1, XPO1, and KRAS. Sole chemotherapy, treatment with Clb-R, or genetic lesions in TP53 (9.9% of patients) and KRAS (6.2% of patients) were significantly associated with nonresponse to study therapy. In multivariate models, complex karyotypes and POT1 mutations (8.1% of patients) represented significant prognostic factors for an unfavorable survival, independently of IGHV mutation status, Binet stage, and serum β-2-microglobuline. Patients with the copresence of complex karyotypes and deletions/mutations involving TP53 demonstrated a particularly short survival. In summary, this is the first prospective, controlled study in CLL patients that shows a role of complex karyotype aberrations as an independent prognostic factor for survival after front-line therapy. Moreover, the study identifies mutations in KRAS and POT1 as novel determinants of outcome after chemoimmunotherapy using chlorambucil and anti-CD20 treatment.
Introduction
Chronic lymphocytic leukemia (CLL) is a clinically heterogeneous B-cell malignancy with a significant level of genomic instability.1,2 Modern high-throughput sequencing technologies have recently tagged a variety of new mutations in genes putatively driving disease onset and progression.2-6 Some of these mutations, in particular in NOTCH1 and SF3B1, have demonstrated significant prognostic value.4,5,7-13 However, their prognostic effect diverges between different studies and has rarely been tested in the context of large, prospective, randomized clinical trials.
Characteristically, CLL cells harbor distinct chromosomal gains or deletions (60-80% of patients), some of which have been identified as important determinants of patient outcome.1,14-17 In clinical routine, the most common aberrations, ie, deletions in chromosome 11q22 [del(11q)], 13q14 [del(13q)], 17p13 [del(17p)], and trisomy 12 [tri(12)], are assessed by fluorescence in- situ hybridization (FISH). However, chromosomal aberrations other than those detected by standard FISH panels may also affect the disease biology and prognosis. We and others have previously described that the presence of chromosomal translocations and cytogenetic complexity (≥3 aberrations detected by karyotype analysis) may be associated with a shortened treatment-free and overall survival (OS) after chemotherapy.14,15,17,18 Recently, the prognostic value of complex karyotypes was also demonstrated in CLL patients treated with ibrutinib, where this parameter showed stronger effects on outcome than del(17p).18
Metaphase karyotyping to assess chromosomal lesions beyond the scope of standard FISH is time consuming. In addition, culture of CLL cells in vitro needs to be optimized for metaphase cytogenetics by using specific coculture conditions.19-21 Therefore, only few centers have adopted this method for routine diagnostics, and this parameter has not been included in clinical trials. To date, prospective clinical data to address the prognostic value of karyotypic findings in the context of current standard therapies, in particular chemoimmunotherapy, have been entirely missing.
Therefore, we aimed to clarify the prognostic role of chromosomal translocations, complex karyotypes, and recurrent gene mutations in a prospective trial using chemoimmunotherapy in CLL patients with relevant comorbidity.22
To this end, we performed a comprehensive genetic analysis using classical metaphase karyotyping and targeted next-generation sequencing (NGS) of an 85-gene panel in 161 CLL patients uniformly treated within the CLL11 study. This trial showed that chemoimmunotherapy with chlorambucil plus CD20-antibody treatment was superior to chlorambucil monotherapy (Clb) and that combined chlorambucil-obinutuzumab (Clb-G) was superior to chlorambucil-rituximab (Clb-R) in previously untreated CLL patients with significant comorbidity.23,24 This allowed to analyze both the value of chromosomal and molecular genetic aberrations in the context of a comprehensive dataset from a uniformly treated population of CLL patients.
Patients, materials, and methods
Patients and treatment
Between 2010 and 2012, 781 patients were included in the CLL11 trial. The study was registered at US and EU clinical trial registries (NCT01010061/EudraCT2009-012476-28) and approved by ethical review boards responsible for each participating center. Only previously untreated patients in need of therapy and coexisting medical conditions (evaluated by the Cumulative Illness Rating Scale [CIRS]) or a creatinine clearance <70 mL/min were included. From 161 patients, baseline peripheral blood samples, shipped within 48 hours to central laboratories in Germany, were collected after patient consent had been obtained. The study was performed according to the principles outlined in the Declaration of Helsinki.
Conventional karyotyping
Fresh peripheral whole blood was cultured in Panserin 411S media (Pan-Biotech, Aidenbach, Germany) under 3 stimulatory conditions: (A) 48 hours or (B) 72 hours in presence of 1 µM CpG-oligodeoxynucleotides (TibMolBiol, Berlin, Germany) and 100 U/mL interleukin-2 (Biochrom, Berlin, Germany), or (C) 48 hours in presence of 0.1 µg/mL tetradecanoyl-phorbolacetate (Sigma-Aldrich, St. Louis, MO). For metaphase arrest, colcemid was added at 200 ng/mL for 1.5 hours (culture A) or at 55 ng/mL (culture B/C) overnight. After hypotonic treatment, cell suspensions were fixed with 3:1 methanol acetic acid and dropped for metaphase spreading on glass slides. After trypsinization and Giemsa staining, karyotypes were analyzed according to the International System for Human Cytogenetic Nomenclature 2013.
NGS
Genomic DNA was purified from CD19-positively selected CLL B cells (Miltenyi Biotec, Bergisch-Gladbach, Germany) using standard columns (Qiagen, Hilden, Germany). Due to limited blood volume, peripheral blood mononuclear cells were used for DNA extraction in 62 cases. Two customized gene panels using the TruSeq amplicon-based technology from Illumina (San Diego, CA; panel A) and the bait capture based SureSelect method from Agilent (Santa Clara/CA; panel B), respectively, were designed and target libraries prepared according to the manufacturer’s instructions (for details, please see supplemental Materials, available on the Blood Web site). Panel A used customized oligonucleotide probes for 563 amplicons to amplify a complete coding or hotspot library from 35 genes (76 kb). For panel B, SureSelect target enrichment was performed capturing a 313-kb panel with 56 genes. Cluster amplification and sequencing was performed on a HiSeq2000 or HiSeq2500 instrument, respectively, using v3 chemistry (Illumina). Variants with insufficient sequence quality were validated by Sanger sequencing, 454 pyrosequencing (GS Junior; Roche, Mannheim, Germany), and/or locked nucleic acid clamp-mediated polymerase chain reaction (supplemental Methods).
Additional laboratory analyses and clinical data collection
Interphase FISH of common chromosomal lesions, IGHV mutation analysis, the analysis of serum parameters (thymidine kinase, β-2-microglobuline [β2M]), and immunophenotyping by flow cytometry were performed as described previously.23,25 The CLL11 trial was initiated collaboratively between the German CLL Study Group (GCLLSG) and F. Hoffmann-La Roche with legal sponsorship taken by the company. Clinical data including routine laboratory parameters, response assessment, and follow-up of remission status and survival were gathered according to trial requirements in the clinical database managed by the sponsor and reviewed by the GCLLSG.
NGS data analysis
Sequence data were analyzed within the Sequence Pilot SeqNext software environment (panel A; JSI Medical Systems, Boston, MA) or the Varbank pipeline v.2.3 developed by the Cologne Center of Genomics (panel B; CCG, Cologne, Germany; supplemental Methods). Raw sequence data (accessible via http://www.cll-research.org/) were processed according to the SeqNext software setup (panel A) or stepwise algorithms (panel B) using the Burrows-Wheeler aligner26 and “The Genome Analysis Toolkit (GATK v1.6).27 We filtered for high-quality variants with a variant allele frequency ≥5% and a minor allele frequency <0.01 based on information provided by dbSNP (build 134),28 the 1000 Genomes database (build 201410),29 the Exome Variant Server (build ESP6500),30 the Exome Aggregation Consortium (ExAc 0.3),31 and COSMIC.32 Only variants predicted to be “deleterious,” “damaging,” or “disease causing” due to associated functional changes at the protein level or due to their occurrence in conserved regions were considered for final analysis (supplemental Methods).
Statistics
We used standard statistical means to evaluate associations between clinical and molecular patient characteristics (χ2/Fisher’s exact; Mann-Whitney/Kruskal-Wallis). Associations of treatment response with distinct patient subsets were evaluated by logistic regression. Time-to-event parameters were estimated by the Kaplan-Meier method and survival curves were compared via the log-rank test. Parameters selected from univariate Cox regression analyses were included into multivariate Cox proportional hazards models using both stepwise forward and backward selection for optimization. All tests were 2 sided, and a P value <.05 was defined as statistically significant. Due to the primarily exploratory purpose of our analysis, no adjustments for multiple tests were performed. Statistical analyses were performed with SPSS v23 (SPSS, Chicago, IL).
Results
Patient characteristics
Between May 2010 and June 2012, we obtained pretreatment peripheral blood for conventional karyotyping and NGS from 161 CLL patients registered for CLL11 (Table 1). There were 56 women (34.8%) and 105 men (65.2%) at a median age of 75 years and a median total CIRS score of 8 (range, 0-18),33 who presented at median 35.6 months from first diagnosis (range, 0.2-269.2 months). Treatment with Clb (24 patients/14.9%), Clb-R (68 patients/42.2%) or Clb-G (69 patients/42.9%) was initiated within 0 to 125 days after sample acquisition. Our analyzed patient set was representative for the complete trial population (781 patients), except for inclusion of more elderly (>70 years) patients (75.2% vs 58.1% in entire cohort) and a slightly increased proportion with trisomy 12 (25.3% vs 17.7% in entire cohort).23
Patient characteristics
| Baseline characteristic . | CLB (n = 24) . | CLB+R (n = 68) . | CLB+G (n = 69) . | Total (n = 161) . |
|---|---|---|---|---|
| Median time since diagnosis (median/range in months) | 50.4 | 31.9 | 30.6 | 35.6 |
| (0.5-269.2) | (0.2-215.2) | (0.2-269.0) | (0.2-269.2) | |
| Median age (range) (years) | 73 (48-85) | 74.5 (50-87) | 76 (62-89) | 75 (48-89) |
| >70, n (%) | 16 (66.7) | 52 (76.5) | 53 (76.8) | 121 (75.2) |
| >80, n (%) | 3 (12.5) | 8 (11.8) | 8 (11.6) | 19 (11.8) |
| Sex, n (%) | ||||
| Female | 11 (45.8) | 24 (35.3) | 21 (30.4) | 56 (34.8) |
| Male | 13 (54.2) | 44 (64.7) | 48 (69.6) | 105 (65.2) |
| Binet stage, n (%) | ||||
| A | 6 (25.0) | 17 (25.0) | 15 (21.7) | 38 (23.6) |
| B | 6 (25.0) | 20 (29.4) | 26 (37.7) | 52 (32.3 |
| C | 12 (50.0) | 31 (45.6) | 28 (40.6) | 71 (44.1) |
| Median total CIRS score (range) | 7 (0-18) | 8 (3-13) | 8 (1-18) | 8 (0-18) |
| Median WBC (range) (×103/µL) | 187.2 | 69.7 | 74.5 | 80.7 |
| (17.6-302.1) | (0.1-365.3) | (3.1-345.6) | (0.1-365.3) | |
| IGHV mutational status, N = 157, n (%) | ||||
| Unmutated | 15 (65.2) | 42 (62.7) | 40 (59.7) | 97 (61.8) |
| Mutated | 8 (34.8) | 25 (37.3) | 27 (40.3) | 60 (38.2) |
| CD38 expression, n (%) | ||||
| Negative (<30%) | 12 (50.0) | 34 (50.0) | 44 (63.8) | 90 (55.9) |
| Positive (≥30%) | 12 (50.0) | 34 (50.0) | 25 (36.2) | 71 (44.1) |
| ZAP-70 expression, n (%) | ||||
| Negative (<20%) | 9 (37.5) | 39 (57.4) | 43 (62.3) | 91 (56.5) |
| Positive (≥20%) | 15 (62.5) | 29 (42.6) | 26 (37.7) | 70 (43.5) |
| s-TK (U/L), N = 159, n (%) | ||||
| ≤10.0 | 10 (43.5) | 29 (42.6) | 31 (45.6) | 70 (44.0) |
| >10.0 | 13 (56.5) | 39 (57.4) | 37 (54.4) | 89 (56.0) |
| s-β2M (mg/L), N = 160, n (%) | ||||
| ≤3.5 | 12 (52.2) | 38 (55.9) | 43 (62.3) | 93 (58.1) |
| >3.5 | 11 (47.8) | 30 (44.1) | 26 (37.7) | 67 (41.9) |
| Hierarchical model by FISH, N = 154, n (%)* | ||||
| Del(17p) | 5 (20.8) | 0 (0.0) | 6 (9.1) | 11 (7.1) |
| Del(11q) | 3 (12.5) | 12 (18.8) | 8 (12.1) | 23 (14.9) |
| Tri(12) | 6 (25.0) | 17 (26.6) | 11 (16.7) | 34 (22.1) |
| Normal | 3 (12.5) | 13 (20.3) | 21 (31.8) | 37 (24.0) |
| Sole del(13q) | 7 (29.2) | 22 (34.4) | 20 (30.3) | 49 (31.8) |
| Conventional karyotyping, N = 154, n (%) | ||||
| Median number of aberrations (range) | 1 (0-7) | 1 (0-6) | 1 (0-8) | 1 (0-8) |
| 0 aberration | 6 (30.0) | 14 (21.2) | 28 (41.2) | 48 (31.2) |
| ≥1 aberration | 14 (70.0) | 52 (78.8) | 40 (58.8) | 106 (68.8) |
| ≥3 aberrations (complex aberrant) | 6 (30.0) | 9 (13.6) | 15 (22.1) | 30 (19.5) |
| Baseline characteristic . | CLB (n = 24) . | CLB+R (n = 68) . | CLB+G (n = 69) . | Total (n = 161) . |
|---|---|---|---|---|
| Median time since diagnosis (median/range in months) | 50.4 | 31.9 | 30.6 | 35.6 |
| (0.5-269.2) | (0.2-215.2) | (0.2-269.0) | (0.2-269.2) | |
| Median age (range) (years) | 73 (48-85) | 74.5 (50-87) | 76 (62-89) | 75 (48-89) |
| >70, n (%) | 16 (66.7) | 52 (76.5) | 53 (76.8) | 121 (75.2) |
| >80, n (%) | 3 (12.5) | 8 (11.8) | 8 (11.6) | 19 (11.8) |
| Sex, n (%) | ||||
| Female | 11 (45.8) | 24 (35.3) | 21 (30.4) | 56 (34.8) |
| Male | 13 (54.2) | 44 (64.7) | 48 (69.6) | 105 (65.2) |
| Binet stage, n (%) | ||||
| A | 6 (25.0) | 17 (25.0) | 15 (21.7) | 38 (23.6) |
| B | 6 (25.0) | 20 (29.4) | 26 (37.7) | 52 (32.3 |
| C | 12 (50.0) | 31 (45.6) | 28 (40.6) | 71 (44.1) |
| Median total CIRS score (range) | 7 (0-18) | 8 (3-13) | 8 (1-18) | 8 (0-18) |
| Median WBC (range) (×103/µL) | 187.2 | 69.7 | 74.5 | 80.7 |
| (17.6-302.1) | (0.1-365.3) | (3.1-345.6) | (0.1-365.3) | |
| IGHV mutational status, N = 157, n (%) | ||||
| Unmutated | 15 (65.2) | 42 (62.7) | 40 (59.7) | 97 (61.8) |
| Mutated | 8 (34.8) | 25 (37.3) | 27 (40.3) | 60 (38.2) |
| CD38 expression, n (%) | ||||
| Negative (<30%) | 12 (50.0) | 34 (50.0) | 44 (63.8) | 90 (55.9) |
| Positive (≥30%) | 12 (50.0) | 34 (50.0) | 25 (36.2) | 71 (44.1) |
| ZAP-70 expression, n (%) | ||||
| Negative (<20%) | 9 (37.5) | 39 (57.4) | 43 (62.3) | 91 (56.5) |
| Positive (≥20%) | 15 (62.5) | 29 (42.6) | 26 (37.7) | 70 (43.5) |
| s-TK (U/L), N = 159, n (%) | ||||
| ≤10.0 | 10 (43.5) | 29 (42.6) | 31 (45.6) | 70 (44.0) |
| >10.0 | 13 (56.5) | 39 (57.4) | 37 (54.4) | 89 (56.0) |
| s-β2M (mg/L), N = 160, n (%) | ||||
| ≤3.5 | 12 (52.2) | 38 (55.9) | 43 (62.3) | 93 (58.1) |
| >3.5 | 11 (47.8) | 30 (44.1) | 26 (37.7) | 67 (41.9) |
| Hierarchical model by FISH, N = 154, n (%)* | ||||
| Del(17p) | 5 (20.8) | 0 (0.0) | 6 (9.1) | 11 (7.1) |
| Del(11q) | 3 (12.5) | 12 (18.8) | 8 (12.1) | 23 (14.9) |
| Tri(12) | 6 (25.0) | 17 (26.6) | 11 (16.7) | 34 (22.1) |
| Normal | 3 (12.5) | 13 (20.3) | 21 (31.8) | 37 (24.0) |
| Sole del(13q) | 7 (29.2) | 22 (34.4) | 20 (30.3) | 49 (31.8) |
| Conventional karyotyping, N = 154, n (%) | ||||
| Median number of aberrations (range) | 1 (0-7) | 1 (0-6) | 1 (0-8) | 1 (0-8) |
| 0 aberration | 6 (30.0) | 14 (21.2) | 28 (41.2) | 48 (31.2) |
| ≥1 aberration | 14 (70.0) | 52 (78.8) | 40 (58.8) | 106 (68.8) |
| ≥3 aberrations (complex aberrant) | 6 (30.0) | 9 (13.6) | 15 (22.1) | 30 (19.5) |
According to Döhner et al.1
NGS identifies alterations in genes known and new to be mutated in CLL
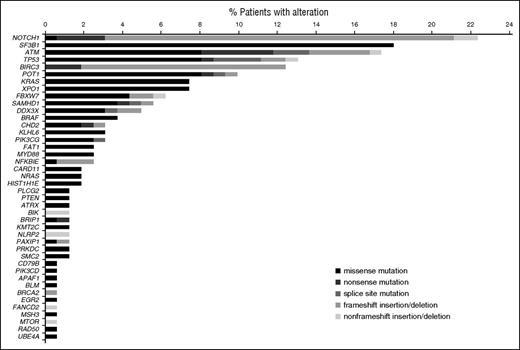
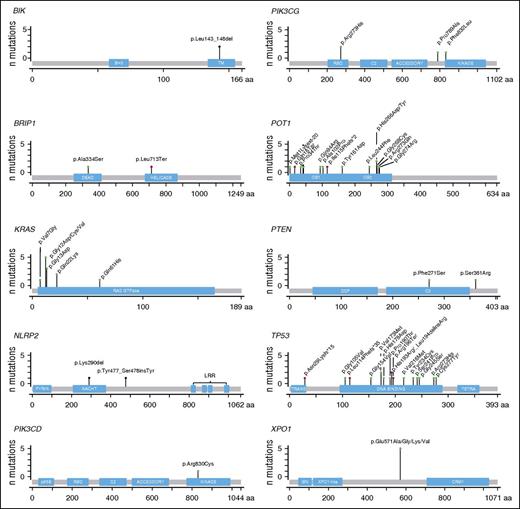
In 42 of 85 distinct genes, NGS identified 187 predominantly heterozygous coding missense or nonsense point mutations, 11 splice site mutations, and 76 insertions/deletions, 86% of which resulted in frameshifts (supplemental Tables 1 and 2). Overall, 123 patients (76.4%) carried ≥1 mutation, and 68 (42.2%) had ≥2 genes affected. Among the most frequently altered genes were targets previously reported to be mutated in CLL, such as NOTCH1 (32 patients/19.9%), SF3B1 (25 patients/15.5%), ATM (20 patients/12.4%), TP53 (16 patients/9.9%), BIRC3 (15 patients/9.3%), POT1 (13 patients/8.1%), XPO1 (12 patients/7.5%), and KRAS (10 patients/6.2%) (Figures 1 and 2). New mutations in genes previously not described in CLL were found in the catalytic subunits of the phosphatidylinositol-4,5-bisphosphate 3-kinases (PIK3CG, 5 patients; PIK3CD, 1 patient), in NLRP2 (2 patients, nucleotide-binding domain and leucine-rich repeat-containing family, pyrin domain containing 2), BIK (2 patients, BCL2-interacting killer), PTEN (2 patients, phosphatase and tensin homolog), and BRIP1 (2 patients, BRCA1 interacting protein C-terminal helicase 1) (Figure 3). Mutations in ATM, KRAS, NOTCH1, SF3B1, and XPO1 were associated with ≥1 unfavorable prognostic feature, ie, an unmutated IGHV status, ZAP70 or CD38 positivity, or elevated serum β2M (Table 2). Only TP53 mutations significantly coincided with the presence of del(17p): 10 of overall 11 cases/7.1% of patients with del(17p) were TP53 mutated (P < .001). Patients with del(11q) (25 patients, 16.1%) carried significantly more mutations in ATM (10 cases; P < .001), BRAF (3 cases; P = .03), and NFKBIE (3 cases; P = .013) than patients without del(11q). A significant enrichment was also seen for BIRC3 (12 cases; P < .001) or FBXW7 (6 cases; P = .017) alterations in overall 39 patients (25.3%) carrying a tri(12). In contrast, the presence of tri(12) was mutually exclusive with mutations in TP53 (P = .012) or in POT1 (P = .039). Similarly, KRAS mutated CLL were exclusively IGHV unmutated but not IGHV mutated (P = .014). Further, KRAS mutations did not coincide with TP53 lesions or complex karyotypes (not significant).
Frequency and type of mutations per gene. Mutations and mutation subtype detected in 42 of 85 genes investigated by targeted NGS in 161 patients treated and followed in the CLL11 study.
Frequency and type of mutations per gene. Mutations and mutation subtype detected in 42 of 85 genes investigated by targeted NGS in 161 patients treated and followed in the CLL11 study.
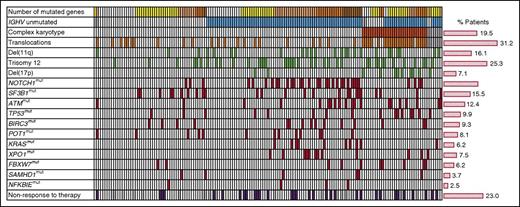
Genetic profiles and treatment response of patients. Each column represents 1 patient (n = 161) and each row 1 particular genetic parameter or treatment response (last row). The histogram on the right summarizes the % frequency of patients who presented with the row parameter in our study cohort. Color code: gray, parameter not available; white, parameter not present; any other color, parameter present. First row (number of mutated genes): white = 0 genes mutated; yellow = 1 gene mutated; light orange = 2 genes mutated; orange = 3 genes mutated; brown = 4 and more genes mutated.
Genetic profiles and treatment response of patients. Each column represents 1 patient (n = 161) and each row 1 particular genetic parameter or treatment response (last row). The histogram on the right summarizes the % frequency of patients who presented with the row parameter in our study cohort. Color code: gray, parameter not available; white, parameter not present; any other color, parameter present. First row (number of mutated genes): white = 0 genes mutated; yellow = 1 gene mutated; light orange = 2 genes mutated; orange = 3 genes mutated; brown = 4 and more genes mutated.
Protein and protein-subdomain localization of mutations/indels in genes previously undescribed in CLL or associated with prognosis. x-axis: length of the protein in amino acids (aa); y-axis: number of mutations at a given protein position. Blue boxes represent important subdomains or motifs of each protein (modified according to MutationMapper v1.0.1).52 Red pins, nonsense or frameshift alterations; green pins, missense mutations; black pins, in-frame alterations.
Protein and protein-subdomain localization of mutations/indels in genes previously undescribed in CLL or associated with prognosis. x-axis: length of the protein in amino acids (aa); y-axis: number of mutations at a given protein position. Blue boxes represent important subdomains or motifs of each protein (modified according to MutationMapper v1.0.1).52 Red pins, nonsense or frameshift alterations; green pins, missense mutations; black pins, in-frame alterations.
Associations between chromosomal or gene alterations, baseline characteristics, and treatment response
| Parameter . | Age . | Binet C vs A/B . | Unmut. IGHV . | ZAP70 ≥20% . | CD38 ≥30% . | β2M >3.5 mg/L . | Del(11q)* . | Del(13q)* . | Del(17p)* . | Tri(12)* . | Chromosomal translocations . | Complex karyotypes . | Nonresponse to therapy . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ATMmut | ∅ | ∅ | .002↑ | ∅ | ∅ | ∅ | <.001↑ | ∅ | ∅ | .045↓ | .014↑ | ∅ | ∅ |
| BIRC3mut | .044↓ | .048↓ | ∅ | ∅ | ∅ | ∅ | (.070)↑ | ∅ | ∅ | <.001↑ | ∅ | ∅ | ∅ |
| BRAFmut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .030↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| CHD2mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| DDX3Xmut | ∅ | ∅ | ∅ | (.079)↑ | ∅ | (.069)↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| FAT1mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| FBXW7mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | (.098)↓ | ∅ | .017↑ | ∅ | .025↑ | ∅ |
| KRASmut | ∅ | ∅ | .014↑ | .021↑ | .005↑ | ∅ | ∅ | (.098)↓ | ∅ | ∅ | (.058)↓ | ∅ | .015↑ |
| MYD88mut | (.066)↓ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| NFKBIEmut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .013↑ | (.057)↑ | ∅ | ∅ | ∅ | ∅ | ∅ |
| NOTCH1mut | (.057)↑ | ∅ | <.001↑ | <.001↑ | .006↑ | .025↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| PIK3CGmut | (.097)↑ | (.067)↓ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| POT1mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .039↓ | ∅ | (.074)↓ | ∅ |
| SAMHD1mut | ∅ | ∅ | ∅ | (.086)↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| SF3B1mut | ∅ | ∅ | ∅ | .024↑ | .009↑ | ∅ | ∅ | (.088)↓ | ∅ | ∅ | .037↓ | ∅ | ∅ |
| TP53mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | <.001↑ | .012↓ | (.072)↑ | .011↑ | .001↑ |
| XPO1mut | .040↓ | ∅ | .030↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| Chromosomal translocations | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .002↑ | ∅ | NA | <.001↑ | ∅ |
| Complex karyotypes | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | <.001↑ | ∅ | <.001↑ | NA | ∅ |
| Nonresponse to therapy | ∅ | ∅ | .007↑ | ∅ | ∅ | ∅ | ∅ | ∅ | .004↑ | ∅ | ∅ | ∅ | NA |
| Parameter . | Age . | Binet C vs A/B . | Unmut. IGHV . | ZAP70 ≥20% . | CD38 ≥30% . | β2M >3.5 mg/L . | Del(11q)* . | Del(13q)* . | Del(17p)* . | Tri(12)* . | Chromosomal translocations . | Complex karyotypes . | Nonresponse to therapy . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ATMmut | ∅ | ∅ | .002↑ | ∅ | ∅ | ∅ | <.001↑ | ∅ | ∅ | .045↓ | .014↑ | ∅ | ∅ |
| BIRC3mut | .044↓ | .048↓ | ∅ | ∅ | ∅ | ∅ | (.070)↑ | ∅ | ∅ | <.001↑ | ∅ | ∅ | ∅ |
| BRAFmut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .030↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| CHD2mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| DDX3Xmut | ∅ | ∅ | ∅ | (.079)↑ | ∅ | (.069)↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| FAT1mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| FBXW7mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | (.098)↓ | ∅ | .017↑ | ∅ | .025↑ | ∅ |
| KRASmut | ∅ | ∅ | .014↑ | .021↑ | .005↑ | ∅ | ∅ | (.098)↓ | ∅ | ∅ | (.058)↓ | ∅ | .015↑ |
| MYD88mut | (.066)↓ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| NFKBIEmut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .013↑ | (.057)↑ | ∅ | ∅ | ∅ | ∅ | ∅ |
| NOTCH1mut | (.057)↑ | ∅ | <.001↑ | <.001↑ | .006↑ | .025↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| PIK3CGmut | (.097)↑ | (.067)↓ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| POT1mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .039↓ | ∅ | (.074)↓ | ∅ |
| SAMHD1mut | ∅ | ∅ | ∅ | (.086)↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| SF3B1mut | ∅ | ∅ | ∅ | .024↑ | .009↑ | ∅ | ∅ | (.088)↓ | ∅ | ∅ | .037↓ | ∅ | ∅ |
| TP53mut | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | <.001↑ | .012↓ | (.072)↑ | .011↑ | .001↑ |
| XPO1mut | .040↓ | ∅ | .030↑ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ |
| Chromosomal translocations | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | .002↑ | ∅ | NA | <.001↑ | ∅ |
| Complex karyotypes | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | ∅ | <.001↑ | ∅ | <.001↑ | NA | ∅ |
| Nonresponse to therapy | ∅ | ∅ | .007↑ | ∅ | ∅ | ∅ | ∅ | ∅ | .004↑ | ∅ | ∅ | ∅ | NA |
Serum TK levels >10 U/L were not significantly associated with any mutation or chromosomal translocations/complex karyotypes and are therefore not included in this overview.
Arrows, direction of the association, eg, BIRC3 mutations are decreased in patients with higher median age; mut, mutation; NA, not applicable; ∅, absence of a statistically significant association (P < .05) or trend (P < .10; in parentheses) per χ2, Fisher’s exact test, or logistic regression (for nonresponse).
Detected by FISH.
Complex karyotypes and chromosomal translocations coincide with TP53 deficiency and mutations in ATM or FBXW7
Stimulatory cell cultures successfully obtained metaphase spreads for karyotyping in 154 cases. One hundred six patients (68.8%) presented with an aberrant karyotype as assessed by metaphase cytogenetics (range, 1-8; Table 1; supplemental Table 3). Combining results obtained by either FISH or karyotyping (n = 161), 139 patients (86.3%) had ≥1 chromosomal abnormality, 123 (76.4%) had aberrations commonly recurring in CLL [ie, del(6q), del(11q), del(13q), del(17p), tri(12)].
Forty-seven patients (30.5%) had ≥1 translocation of chromosomal material (includes 18 patients with solely balanced, 19 with solely unbalanced, and 10 with both types of translocations) and 30 patients (19.5%) exhibited complex karyotypes (≥3 chromosomal aberrations). In the 47 cases carrying translocations (any type, balanced, or unbalanced), we found a significant enrichment of complex karyotypes (25 cases/52.1%, P < .001), del(17p) (8 cases/17.0%, P = .002) and of mutations (11 cases/22.9%, P = .004) but not deletions in ATM (Table 2). The most common translocation breakpoints involved chromosome band 14q32 (10 cases), followed by 8q24 (5 cases), 13q12 (4 cases), 15q15 (4 cases), and 19p13 (4 cases). Another interesting finding was that high levels of chromosomal instability, as indicated by complex karyotypes in 30 patients were associated with the presence of mutations in the ubiquitin ligase FBXW7 (5 cases/16.7%, P = .025) or with genetic lesions involving TP53 [del(17p) and/or TP53 mutation in 8 cases/26.7%, P = .005].
TP53 deficiency and KRAS mutations associate with nonresponse to Clb-based chemo- and/or chemoimmunotherapy
We evaluated clinical and molecular features present at baseline and their associations with response to Clb-based front-line therapy and time-to-event outcome after randomization. Overall, patients received a median number of 6 treatment cycles (range, 1-6). Response assessment at 3 months after the end of treatment according to international workshop on CLL (iwCLL) criteria34 was available in 139 patients, of whom 107 (77.0%) obtained at least a partial remission. Thirty-two patients (23.0%) did not respond to Clb (13 patients), Clb-R (14 patients), or Clb-G (5 patients). As described in the main trial, addition of anti-CD20 therapy, in particular of obinutzumab, significantly decreased the risk of nonresponse to therapy in our patient cohort (supplemental Table 4). On a molecular level, an unmutated IGHV (odds ratio [OR], 4.1, 95% confidence interval [CI], 1.5-11.6; P = .007) and the presence of del(17p) (OR, 8.3; 95% CI, 1.9-35.4; P = .004) were associated with nonresponse to therapy (Figure 2; Table 2; supplemental Table 4). Of 32 nonresponders, 8 patients (31.3%) were TP53 mutated (4 Clb, 2 Clb-R, 2 Clb-G treated), 6 of these (18.8%) showed an additional del(17p) (3 Clb, 3 Clb-G treated). Interestingly, 5 nonresponders to chemoimmunotherapy carried a KRAS exon 2/3 mutation (15.6%; 1 Clb, 4 Clb-R treated). Together, TP53 deficiency was associated with nonresponse to both chemo- and chemoimmunotherapy (OR, 7.1; 95% CI, 2.1-23.6; P = .002), whereas KRAS mutations predominantly correlated with nonresponse to chemoimmunotherapy, in particular Clb-R (OR for entire study, 8.5; 95% CI, 1.7-42.0; P = .008). Four patients (12.5%) were FBXW7 mutated and did not respond to Clb-R (3 cases) or Clb-G (1 case, P = .026). However, 1 of these cases carried an additional del(17p), and 1 patient was KRAS mutated, suggesting that mutant FBXW7 was not the only genetic lesion driving this phenotype. Other mutations, complex karyotypes or chromosomal translocations did not affect the response to therapy (Figure 2; Table 2; supplemental Table 4).
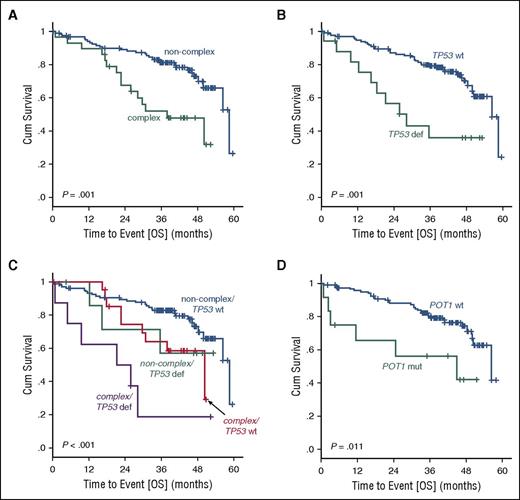
Complex karyotypes and mutated POT1 impact OS after Clb-based chemo- or chemoimmunotherapy
After a median observation time of 40.9 months (range, 0-59.6 months), an overall of 114 events for progression-free survival (PFS) and 49 events for OS were available. Based on univariate comparison, sole chemotherapy (Clb), elevated serum β2M, del(17p), del(11q), unmutated IGHV, ZAP70 positivity, and chromosomal translocations were significantly associated with PFS (supplemental Table 4). KRAS and XPO1 mutated cases demonstrated a significantly decreased PFS after chemoimmunotherapy (Clb-R/Clb-G). The parameters age, Binet stage, del(17p), unmutated IGHV, TP53 mutations, and complex karyotypes were correlated with OS. In addition, POT1 mutations were associated with shorter OS in patients receiving Clb-R or Clb-G (hazard ratio [HR], 2.9; 95% CI, 1.2-7.1; P = .011), as all but 1 POT1 mutated patients had been assigned to chemoimmunotherapy (Figure 4; supplemental Table 4).
Kaplan-Meier survival functions for overall survival according to the presence of complex karyotypes, genetic lesions in TP53, or POT1 gene mutations. OS (A) in 30 patients with vs 124 patients without complex karyotypes, (B) in 17 vs 137 patients with deletions or mutations in TP53, (C) or with either one or both of these 2 genetic features present (109 patients with no complex karyotypes and no TP53 hit vs 22 patients with complex karyotypes and no TP53 lesion, vs 8 patients with a TP53 mutation or deletion and no complex karyotype, vs 8 patients with complex karyotypes and a TP53 mutation or deletion). (D) OS in 13 patients with vs 148 patients without POT1 mutations and treated with Clb-G or Clb-R, because all except 1 of 13 patients with POT1 mutations had been assigned to a chemoimmunotherapy study arm. Complex indicates complex karyotypes; noncomplex, absence of complex karyotypes; TP53 def, presence of a deletion or mutation in TP53).
Kaplan-Meier survival functions for overall survival according to the presence of complex karyotypes, genetic lesions in TP53, or POT1 gene mutations. OS (A) in 30 patients with vs 124 patients without complex karyotypes, (B) in 17 vs 137 patients with deletions or mutations in TP53, (C) or with either one or both of these 2 genetic features present (109 patients with no complex karyotypes and no TP53 hit vs 22 patients with complex karyotypes and no TP53 lesion, vs 8 patients with a TP53 mutation or deletion and no complex karyotype, vs 8 patients with complex karyotypes and a TP53 mutation or deletion). (D) OS in 13 patients with vs 148 patients without POT1 mutations and treated with Clb-G or Clb-R, because all except 1 of 13 patients with POT1 mutations had been assigned to a chemoimmunotherapy study arm. Complex indicates complex karyotypes; noncomplex, absence of complex karyotypes; TP53 def, presence of a deletion or mutation in TP53).
In multivariate analysis, entering parameters with a univariate P < .1 (supplemental Table 3), lack of antibody treatment (P ≤ .001), unmutated IGHV (P < .001), and deficient TP53 [del(17p) and/or TP53 mutated; P = .001] were identified as independent factors for PFS (Table 3). For OS, we identified complex karyotypes (HR, 2.7; 95% CI, 1.4-5.3; P = .004) and POT1 mutations (HR, 4.0; 95% CI, 1.6-10.1; P = .003) as variables with significant prognostic value, independently of established markers such as an advanced Binet stage (P < .001), elevated β2M (P = .043), and an unmutated IGHV (P = .003) (Table 3). Both complex karyotypes and mutated POT1 also retained their independent prognostic value, when we limited the multivariate modeling to the patient subset treated with chemoimmunotherapy (Clb-R/Clb-G) (HR for complex karyotypes, 2.6; 95% CI, 1.2-5.7; P = .018; HR for mutated POT1, 5.2; 95% CI, 2.0-13.3; P = .001), independently of Binet stage (P < .001) and an unmutated IGHV (P = .006).
Prognostic factors associated with PFS and OS in multivariate models
| Variable . | HR . | 95% CI . | P value . | |
|---|---|---|---|---|
| Lower . | Upper . | |||
| Multivariate Cox regression for PFS | ||||
| Clb-R vs Clb | 0.385 | 0.217 | 0.684 | .001 |
| Clb-G vs Clb | 0.149 | 0.081 | 0.274 | <.001 |
| Unmutated IGHV | 3.278 | 2.081 | 5.163 | <.001 |
| Del(17p) and/or TP53mut | 3.079 | 1.550 | 6.116 | .001 |
| Multivariate Cox regression for OS | ||||
| β2M >3.5 mg/L | 1.879 | 1.020 | 3.459 | .043 |
| Complex karyotypes | 2.682 | 1.366 | 5.264 | .004 |
| Unmutated IGHV | 3.061 | 1.482 | 6.321 | .003 |
| POT1mut | 3.997 | 1.581 | 10.106 | .003 |
| Binet C vs A/B | 4.251 | 2.193 | 8.240 | <.001 |
| Variable . | HR . | 95% CI . | P value . | |
|---|---|---|---|---|
| Lower . | Upper . | |||
| Multivariate Cox regression for PFS | ||||
| Clb-R vs Clb | 0.385 | 0.217 | 0.684 | .001 |
| Clb-G vs Clb | 0.149 | 0.081 | 0.274 | <.001 |
| Unmutated IGHV | 3.278 | 2.081 | 5.163 | <.001 |
| Del(17p) and/or TP53mut | 3.079 | 1.550 | 6.116 | .001 |
| Multivariate Cox regression for OS | ||||
| β2M >3.5 mg/L | 1.879 | 1.020 | 3.459 | .043 |
| Complex karyotypes | 2.682 | 1.366 | 5.264 | .004 |
| Unmutated IGHV | 3.061 | 1.482 | 6.321 | .003 |
| POT1mut | 3.997 | 1.581 | 10.106 | .003 |
| Binet C vs A/B | 4.251 | 2.193 | 8.240 | <.001 |
The table lists independent variables associated with time-to-event outcome (PFS or OS) in multivariate analysis. Briefly, all parameters with a univariate P < .10 in univariate analysis (supplemental Table 3) were entered into multivariate Cox proportional hazards models to identify variables with significant and independent prognostic value.
Deficient TP53 [del(17p) and/or mutated TP53] did not emerge as an independent parameter in our final models for survival, even when sole del(17p) without TP53 mutations were considered as a variable. Although TP53 lesions significantly coincided with complex karyotypes in our patient set, a statistical interaction between both parameters was not detected (supplemental Table 5), pointing to a TP53-independent value of karyotypic complexity as a prognostic marker. Kaplan-Meier estimates to visualize survival functions of patients with or without complex karyotypes in context of defective TP53 suggested that complex karyotypes alone exhibited an impact on survival similar to sole TP53 lesions. However, the combined occurrence of both complex karyotypes and TP53 lesions resulted in a particularly poor prognosis of patients (P < .001; Figure 4C).
Discussion
CLL patients with a high level of comorbidity are generally considered prone to treatment related toxicity and therefore not eligible to receive aggressive frontline treatment, ie, with fludarabine, cyclophosphamide, and rituximab. The CLL11 trial was the first to investigate less intensive Clb-based chemo- and chemoimmunotherapy in a patient cohort selectively limited to “nonfit” (“slow go”) patients in a randomized phase 3 setting.23,24 In these physically compromised and typically elderly CLL patients very little is known about the specific prognostic value of molecular characteristics including somatic mutations.
We combined here classical chromosome banding, FISH, and targeted NGS to achieve a comprehensive genetic profiling of CLL cells from 161 patients treated in the CLL11 study. Compared with the full patient cohort registered in this multicenter and multinational trial, our study comprises a relatively small subset of patients. This is explained by the fact that for conventional chromosome banding fresh samples needed to be shipped from centers in local proximity to German central laboratories within 48 hours. Despite this limitation, the study generated a significant number of new findings with regard to the relevance of genetic events in CLL.
The study is the first prospective, controlled trial to examine the role of chromosome banding in CLL. In contrast to previous reports, the presence of neither overall nor unbalanced chromosomal translocations detected by chromosome banding was independently associated with a decreased PFS or OS in our patient cohort. This might be explained by the fact that previous studies were performed in patients who were at various disease stages, or received chemotherapy alone, and that fewer parameters were included in multivariate analyses (eg, without considering TP53 mutations).14,17 We found that >50% of affected cases with chromosomal translocations also showed complex karyotype abnormalities. Cytogenetic complexity represented as being associated with a shortened time to retreatment (supplemental Figure 1) and as one of the most significant prognostic factors of poor survival in multivariate analyses, partially overriding the prognostic value of genetic defects in TP53. The strength of karyotypic complexity as a prognostic parameter in our data corroborates findings proposed by several studies using classical and modern (cyto-)genetic technologies in variable, but rarely in uniform or prospective treatment settings of CLL.14,15,18,35-38 The illustration of survival functions according to the presence and absence of complex karyotypes and TP53 lesions suggested a functional synergy between these 2 genetic features resulting in a most detrimental survival outcome in patients, when both of them are present. Similar observations were recently reported by Baliakas et al,37 who obtained karyotype data from 1001 previously untreated CLL cases and found a decreased time-to-first treatment in patients with del(17p) and concomitant complex karyotypes compared with patients with del(17p) alone. A particularly poor survival for patients with complex karyotypes coinciding with TP53 alterations has also been shown in acute myeloid leukemias.39 It remains speculative whether specific chromosomal aberrations, unknown mutations, or other cellular events are responsible for this prognostic effect of complex karyotypes. Also, the copresence of a mono- vs biallelic inactivation of TP53 or other cellular mechanisms resulting in a partial or complete loss of p53 function might have implications here.40 Overall, both complex karyotypes and translocations may classify cases with a higher level of genomic instability and therefore represent prognostically distinct subsets of CLL patients. Along these lines, the categorization of complex karyotypes versus translocations might represent a more acurate assessment of the level of genomic instability, which is at least in part independent of genetic alterations in TP53.
Our study confirmed NOTCH1, SF3B1, ATM, TP53, and BIRC3 as the 5 most commonly mutated genes in CLL patients.2-5 These mutations were followed by alterations in POT1, XPO1, KRAS, FBXW7, DDX3X, SAMHD1, BRAF, CHD2, MYD88, and NFKBIE.2,4,5 The majority of these mutations were previously reported to occur somatically in CLL or other types of cancer indicating that our functional assessment and filtering algorithms were robust and yielded valuable data. For example, all patients classified as NOTCH1 or SF3B1 mutated, as well as 15 of 16 cases found to be TP53 mutated by our analysis, carried ≥1 previously known somatic mutation.
In addition, our study revealed an increased frequency of KRAS mutations in patients not responding to chemoimmunotherapy. Our NGS assay focused on the analysis of KRAS exon 2 and 3, as they represent the most common hotspot of mutations, which prevent guanine triphosphate hydrolysis and result in a sustained activation status of KRAS. Three of the 5 KRAS mutant nonresponding patients carried a typical glycine to aspartate mutation at codon 12 or 13. KRAS, as well as NRAS, belong to the MAPK-ERK signaling pathway, which represents an important effector pathway of the B-cell receptor.41 Large-scale exome/genome sequencing studies have obtained variable frequencies of mutant KRAS, the highest fraction (14 patients, 2.6%) being recently reported in 538 treatment-naive CLL patients.2 In our study, 10 patients (6.2%) carried 12 KRAS missense mutations, 9 of which were detected at a subclonal level <15% and potentially missed by Sanger or exome/genome sequencing. A potential role of KRAS for the resistance toward chemoimmunotherapy with Clb and rituximab is supported by recent findings of Foà et al, who reported an upregulation of KRAS and NRAS mRNA in patients not responding to Clb-R frontline therapy.38
A potential role of the FBXW7 gene for treatment resistance was suggested by our observation that 4 of 19 patients resistant to Clb-R or Clb-G therapy showed FBXW7 mutations. Of these, 2 patients developed an early disease transformation 1 and 3 months after the end of Clb-R therapy, respectively (1 B-cell prolymphocytic leukemia, 1 diffuse large B-cell lymphoma). Both patients died within 12 months after transformation. FBXW7 encodes a tumor suppressive F-box protein, which regulates various oncoproteins (cyclin E, c-myc, notch) by flagging them for ubiquitin-mediated degradation.42 Siu et al showed that disrupted binding of cyclin E to FBXW7 results in chromosomal instability in hematopoietic progenitor cells.43 These findings provide a potential functional link of FBXW7 alterations with complex karyotypes and might explain the rapid disease transformation in FBXW7 mutated cases following chemoimmunotherapy.
In multivariate analyses, only POT1 was retained as a recurrently mutated gene and independent prognostic factor for OS. POT1 plays an important role for the protection of chromosomal telomeres acting as a component of the shelterin complex.44-46 All mutations detected by our panel were located in the DNA-binding OB1-/OB2-domain.47 In contrast to observations made in POT1 mutated cell lines,48 we did not observe an increased presence of chromosomal abnormalities in POT1 mutated CLL cells before first-line treatment was initiated. Further, there was no overlap of POT1 mutations with other prognostic features or a statistic interaction with assigned study treatment. As recently described by Veronese et al, multiple factors might be required to significantly disturb the shelterin complex in a way that it causes shortened telomeres and the acquisition of additional chromosomal aberrations.49 Follow-up studies in POT1 mutated patients could elucidate, whether telomere shortening and increasing chromosomal instability under subsequent therapies might be responsible for the independent prognostic value of this gene mutation for survival.
Although they were associated with established markers of an unfavorable prognosis, mutations in NOTCH1 and SF3B1 did not provide an independent prognostic effect on PFS or OS in our data. An univariate association of NOTCH1 mutations with survival was noted, when only patients treated with Clb-R were analyzed, but not in the Clb or Clb-G arm (data not shown). Similarly, the prognostic effect of mutated NOTCH1 was limited to the fludarabine, cyclophosphamide, and rituximab compared with the FC-study arm in the CLL8 trial.25 Investigation of these gene mutations in the full CLL11 study cohort might clarify whether treatment specific findings can be corroborated in a larger patient set for final conclusions.
We also describe a new set of mutations, which might be rare in CLL, but might influence the disease pathophysiology. For example, 6 mutations occurred in the δ/γ isoforms of the of the PI3 kinase catalytic subunit p110 (PIK3CD and PIK3CG; Figure 2), the target of novel inhibitors such as duvelisib or idelalisib.
Besides ATM, 15 mutations or deletions were retrieved in genes involved in canonical pathways of the DNA damage response, such as homologous recombination and crosslink repair (BLM, BRCA2, BRIP1, FANCD2, PAXIP1, RAD50, ATRX), nonhomologous end-joining (PRKDC), mismatch repair (MSH3), and in the regulation of chromosome stability (SMC2). Two new BRIP1-mutations detected by our NGS panel were located in the dead or helicase domain of the protein, respectively. Due to the importance of an intact helicase domain for the physical interaction of BRIP1 with BRCA1,50 mutations in this region might affect successful homologous recombination of DNA double strand breaks.
Overall, our report presents the first comprehensive, prospective analysis of chromosomal aberrations (including complex karyotype abnormalities), gene mutations, and clinical and biological features in CLL patients with relevant comorbidity that were treated with Clb-based chemo- or chemoimmunotherapy. The study generated ≥4 relevant findings: First, mutated KRAS correlated with nonresponse to chlorambucil-based chemoimmunotherapy, particularly including rituximab. This finding should be considered for further clinical validation and functional studies. Targeting of KRAS mutated patients with MEK, BRAF, or ERK inhibitors or by combined cell cycle checkpoint blockade through simultaneous Chk1 and MK2 inhibition51 might offer personalized treatment strategies to be investigated in such cases. Second, complex karyotype abnormalities were an independent prognostic factor for survival following chemo(immuno)therapy; this effect seemed to occur in synergy with genetic lesions in TP53. Thus, global karyotyping (ie, by chromosome banding analysis) seems to substantially contribute to the identification of CLL patients with most adverse prognosis and should be considered a standard assessment in future CLL trials. Third, mutations of the POT1 gene were associated with shorter survival in patients receiving Clb-based frontline therapy. Fourth, we found previously unreported mutations located in genes involved in the DNA damage response, which might contribute to the accumulation of genomic alterations and clonal evolution of CLL. Some of these findings await further investigation in clinical trials, in particular those investigating kinase or Bcl-2 inhibitors for CLL.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are indebted to our patients, who provided primary material, and to the clinical investigators (in particular Lothar Müller in Leer, Germany, and Michael Eckart in Erlangen, Germany) for considering patients for the CLL11 trial. The authors thank Agata Jarosz, Christian Becker, and Marek Franitza from the NGS group of the Cologne Center for Genomics for expert technical assistance and Marius Stiefelhagen and Hans Jiro Becker for their assistance with patient sampling at the University of Cologne.
The sequencing and analysis part of this project was supported by the Volkswagenstiftung (Lichtenberg Program) (H.C.R.), Deutsche Forschungsgemeinschaft grant KFO-286 (H.C.R., M. Hallek, M. Herling, K.A.K., P.N., C.D.H.), Deutsche Jose Carreras Leukämie Stiftung grants R12/26 (H.C.R.) and R13/33 (K.A.K.), the Helmholtz-Gemeinschaft (Preclinical Comprehensive Cancer Center) (H.C.R.), Else Kröner-Fresenius Stiftung grant EKFS-2014-A06 (H.C.R.), Deutsche Krebshilfe grants 111724 (H.C.R.) and 111348 (M. Herling), and a local Cologne Excellence Cluster on Cellular Stress Response in Aging-Associated Diseases grant. The clinical study was funded by F. Hoffmann-La Roche.
Authorship
Contribution: C.D.H. designed the project and NGS research panel, analyzed and evaluated the data, supervised the project, and wrote the paper; M.K. designed the diagnostic part of NGS, analyzed and evaluated data, and performed validation experiments; C.K.R. performed the conventional karyotyping; J.A. supported the design of the gene panels, supervised NGS data generation, and together with H.T. analyzed and evaluated NGS data; J.B. and S.K. performed the statistical analysis; G.C. performed the variant annotation and the functional assessment of mutations; M. Herling performed immunophenotyping and analyzed data; J.S. reviewed immunophenotype data; A.E. performed medical review of clinical data; E.T. and H.D. coordinated central genetic diagnostics including cell purification, FISH, and IGHV mutation analysis; V.G. and K.F. coordinated the clinical trial and were responsible for the clinical data collection; S.S. supervised central genetic diagnostics and provided diagnostic results and samples; P.N. supervised the NGS facility; H.C.R. provided expert advice and designed/supervised the project; M. Hallek initiated and designed the project, provided infrastructure for the entire project, designed and conducted the clinical trial (CLL11 study), supervised the project, and wrote the paper; and K.A.K. designed the project, provided samples, performed immunophenotyping and karyotyping, analyzed data, supervised the project, and wrote the manuscript.
Conflict-of-interest disclosure: K.A.K, M. Hallek, and S.S. received research funding from F. Hoffman-La Roche. Additional support by F. Hoffmann-La Roche was received in context of the full CLL11 trial by A.E., K.F. (travel grants), and V.G. (speaker’s honorary, compensation for advisory board and consultancy activities). The remaining authors declare no competing financial interests.
Correspondence: Carmen Diana Herling, Laboratory of Functional Genomics in Lymphoid Malignancies, Department of Internal Medicine I, University of Cologne, Kerpener Strasse 62, 50937 Cologne, Germany; e-mail: carmen.herling@uk-koeln.de.
References
Author notes
C.D.H. and M.K. contributed equally to this study.