Abstract
Introduction: Recent changes in health care financing have increased the out-of-pocket costs borne by families. The potential "financial toxicity" can pose challenges for families beyond those encountered in the treatment of cancer. Several families of children diagnosed with leukemia at our center have recently requested information on the expected costs of the planned treatment. There is little published information on the patient's cost (that is, the health system patient charges) for childhood cancer treatment, and costs can be expected to vary between patients and institutions. To better understand the cost of leukemia treatment at our center, the charges accumulated over the course of therapy for a cohort of children with acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) were analyzed.
Methods: A sample of children who successfully completed treatment at our institution in 2014 using the current Children's Oncology Group (COG) treatment protocols for standard risk ALL (AALL0932) and AML (AAML0531) was chosen. All inpatient and outpatient charges for the entire course of therapy for each child were used to determine total charges for treatment and types of charges (room and board, medications, laboratory, radiology, professional fees). Using our health system's chargemaster data, the expected charges for ALL therapy based upon protocol requirements was estimated and compared to actual charges. We analyzed high frequency and high cost items to identify potential drivers of charges to suggest areas for potential cost reduction.
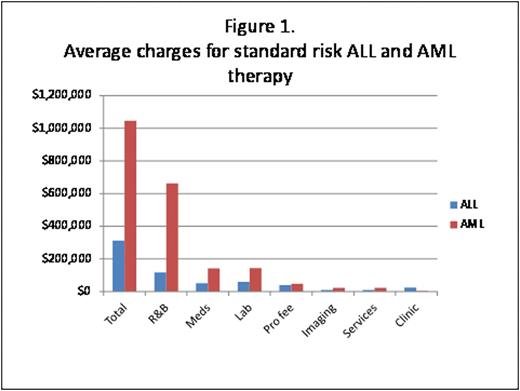
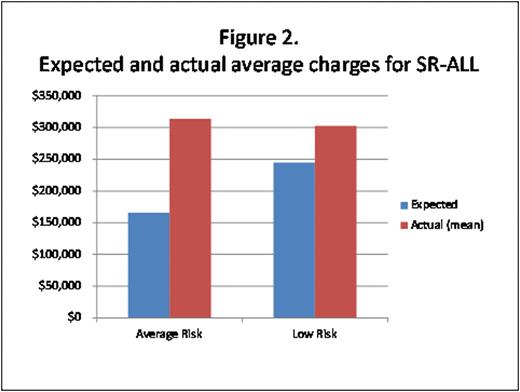
Results: Charges for 11 patients with ALL and 7 with AML were assessed. The average charges for ALL therapy were $311,000 (range $182,000-634,000) and for AML were $1.05 million (range $733,000-$1,346,000). For ALL, room and board, medications, and laboratory accounted for 37%, 16%, and 19% of charges respectively. For AML, room and board medications and laboratory accounted 66%, 14%, and 14% of charges respectively. (Figure 1) Low risk ALL treatment had higher overall charges driven by increased inpatient chemotherapy. Expected charges for low risk ALL treatment were $245,000 compared to $165,000 for average risk standard therapy. Actual charges however did not differ greatly between low risk and average risk ALL subtypes. (Figure 2) The highest charges for items in ALL therapy were for intravenous immune globulin (IVIG), asparaginase, and inpatient stays (intensive care and oncology ward). For AML, the most expensive items were inpatient stays (intensive care and oncology ward), blood products, and complete blood counts (CBC).
Conclusion: AML therapy is more expensive than ALL therapy, driven primarily by the prolonged hospitalizations awaiting count recovery after each cycle. ALL treatment charges were highly variable depending upon experienced toxicities and arm of therapy. Low risk therapy for ALL has the potential to be the most expensive ALL therapy due to six inpatient courses of intermediate dose methotrexate. Estimates for ALL therapy charges did not capture medical toxicity expense or other supportive care related charges. Many drivers of cost cannot be altered without affecting quality of care, but increasing outpatient therapy has the potential to provide the largest reduction in charges. The use of IVIG in some ALL patients and the frequency of CBCs in AML patients highlighted areas where clinical interventions could be implemented without obvious decrements to care quality and with potential cost savings. Understanding data on patient charges can provide an expected range of charges for families and may inform areas to target for cost savings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal