Abstract
Background
Although allogeneic hematopoietic stem cell transplantation (alloSCT) is a curative option to treat hematologic malignancies, disease recurrence remains a concern in the setting of high risk diseases. Thus, post alloSCT therapeutic strategies are needed to treat and/or prevent disease progression. In this setting, donor lymphocytes infusion (DLI) is an option as post alloSCT immunotherapy aiming to enhance graft versus leukemia (GVL) effect. Although DLI may induce persistent remission, graft versus host disease (GVHD) is a potential complication following DLI. Because of the suspected higher incidence of GVHD in the presence of HLA mismatches, few series focused on DLI following haploidentical stem cell transplantation (HaploSCT) so far. We therefore report our experience of DLI following HaploSCT using post-transplantation cyclophosphamide (PT-Cy) platform.
Methods:
We included in this single center study all consecutive adult patients with hematological malignancies who received DLI after HaploSCT with PT-Cy as part of GVHD prophylaxis from 2013 to 2016 (n=21). Conditioning regimens were non-myeloablative (low dose TBI-based) or with reduced toxicity (various dose of busulfan according to disease and patient characteristics). Ciclosporine A and mycophenolate mofetil were given as additional GVHD prophylaxis in all cases. DLI were given at escalating doses, expressed as CD3+cells/kg, without GVHD prophylaxis, and ranged from 1x105 to 5x107 cells/kg.
Results:
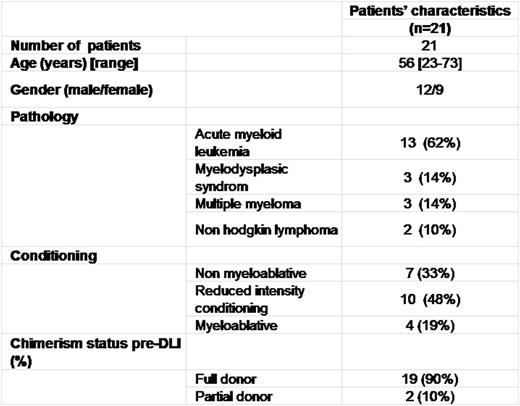
Eleven patients (52%) were transplanted for high risk disease according to the disease risk index (DRI, Armand et al., blood 2015). Twelve patients (57 %) received haploSCT in complete remission,.18 patients received first transplant and 3 patients their second transplant. After HaploSCT, 21 patients (median age: 56 years [range: 23-73]) received either therapeutic (treatment of hematological post transplantation relapse, n=6) or prophylactic (n=15) DLI. The median interval from HaploSCT to the first DLI was 128 days (range: 79-1011). The average number of DLI per patient was 1.8 (range, 1-3). Clinical characteristics are outlined in Table 1. Patients with AML and MDS received DLI alone (n = 13) or in association with azacytidine (n = 2). Patients with MM received DLI in association with Revlimid (n=3). Chimerism before first DLI was complete in 19 patients. 6 patients (33%) developed post DLI GVHD in a median time of 42 days (range: 30-210) with exclusively chronic features. 2 patients (9 %) had severe forms of chronic GVHD. GVHD-related death occurred in 1 patient No response was achieved when DLI were given as therapeutic and 4 of 6 patients died from disease progression. Otherwise, only 3 of 16 patients who received prophylactic DLI experienced relapse.
With a median follow up of 129 days, overall survival was 63%.
Conclusion
Our study suggests that DLI following HaploSCT with PT-Cy is feasible. GVHD is frequent but with a relatively low incidence of severe forms. No response rate was achieved in the context of hematological relapse, underlining that preemptive or prophylactic strategy might be preferred. Indeed, the overall good outcome in patients receiving prophylactic DLI is promising taking into account the poor prognostic of the diseases indicated for alternative donor transplantation. Further prospective studies are needed in specific disease settings to assess the benefit for using such post alloHSCT immune-intervention.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal