Abstract
Introduction
Patients post allogeneic stem cell transplant (allo SCT) are expected to be at high risk of tuberculosis (TB) due to underlying immunosuppression. The incidence is predicted to be higher in countries endemic to TB, like ours. We conducted a retrospective study of post alloSCT patients for incidence of TB, its clinical presentation, factors associated with TB and its outcome.
Methods
Records of all patients who underwent allo SCT from 1st January 2012 till 31st December 2015 were reviewed for transplant related parameters and tubercular infection. The diagnosis of tuberculosis was considered if Mycobacterium tuberculosis (MTB) cultured from clinical samples or acid fast bacilli (AFB) demonstrated on histopathology/ smears. A possible TB was considered in presence of epitheloid cell granulomas without AFB. Patients already on anti-tubercular therapy (ATT) at the time of SCT or had any history of TB were excluded from study population.
Results
A total of 176 patients underwent allo SCT in study period with one patient having past history of TB lymphadenitis (excluded from further analysis). Indications for allo SCT were malignant diseases and non-malignant diseases in 82.3% (n=144) and 17.7% (n=31) patients respectively. Conditioning regimen was myeloablative in 57.7%(n=101) and reduced intensity in 20.6% (n=36) and non myeloablative in 21.7% (n=38). Total body irradiation (TBI) based myeloablative regimen was used in 24.5% (n=43) of patients. Anti-thymocyte globulin (ATG) was used in 14.8% of conditioning regimen. 19 patients underwent unrelated allotransplants. Overall 94 (53.7%) of patients experienced any graft vs host disease (GvHD) (acute 37% (n=65), chronic 29% (n=51) of all patients). Treatment related mortality in the study population was 26.3% (n=46) and overall survival was 50.3% (n=88) at 345 days of median follow up.
Tuberculosis was detected in 5 patients (3 males, 2 females), none had a history of contact with TB, who underwent allo SCT (related =4, unrelated =1). Peripheral blood was used as graft source in all with myeloablative non TBI based conditioning regimen used in 2 patients while TBI based myeloablative conditioning regimen in 1 patient and reduced intensity conditioning in rest 2 patients. ATG was used in one patient for conditioning. Median ECOG performance score of all the 5 patients was 1 (0-1). Only one patient (diagnosis- acute lymphoblastic leukemia) received steroid based treatment as a part of pre transplant treatment during induction chemotherapy. Four patients developed pulmonary tubercular infection while one had lymph nodal involvement after allogeneic SCT, accounting to an incidence rate of tubercular infection of 2.8% at a median of 258 days post allo SCT. The presenting symptoms for TB were unexplained fever (n=4), weight loss (n=1), chest pain (n=2), cough with expectoration (n=1) which lasted for a median of 20 days till TB diagnosis was confirmed using lung biopsy (n=3), BAL culture (n =1) and lung FNA (n=1).
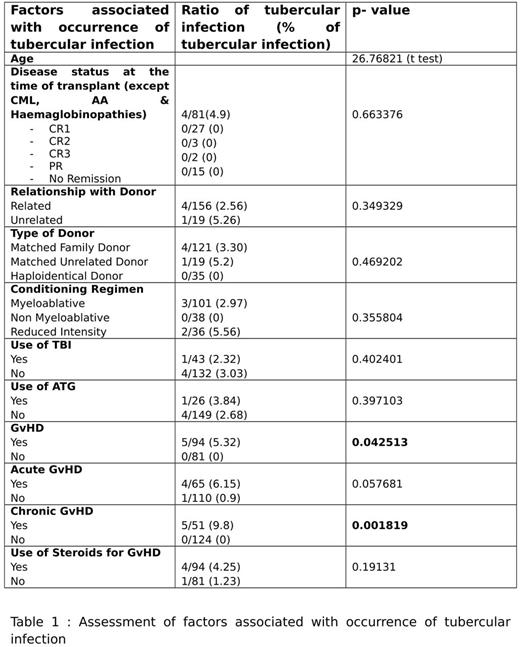
All 5 patients had GvHD in one of its form and four patients who presented with pulmonary disease were receiving median number of 2 (1-3) immunosuppressive therapies at the time of TB diagnosis. Four patients with acute GvHD had received steroids as part of treatment. Presence of any GvHD and chronic GvHD was found to be significantly associated with Tubercular infection (p=0.042) and (p=0.002) respectively as per Fischer exact test. Acute GvHD, though present in 4/5 patients, had a trend towards Tubercular infection (p=0.058) (Table 1).
All patients were started on 4 drug ATT with clinical/ radiological response in all. One patient developed transaminitis post 7 days of start of ATT for which dose modification was done and the other patient developed hyperbiluribinemia, which required temporary cessation of ATT. All the patients who developed TB are alive with a median overall survival of 1071 days post allo SCT.
Conclusion
The incidence of TB is very high amongst allo SCT recipients, as compared to general population. Tuberculosis should be suspected in patients with unexplained fever post allogeneic SCT. Most of cases are pulmonary TB. Active GvHD and ongoing immunosuppression/ steroids are possible risk factors. Early diagnosis and treatment can salvage most of these patients and prevent long term morbidity and mortality. Hepatic toxicity following ATT is common and needs to be differentiated from hepatic GvHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal