Abstract
CONTEXT: Cytomegalovirus reactivation (R-CMV) is often diagnosed in allogeneic hematopoietic cell transplant recipients and could determine a CMV-related disease in these immunocompromised patients, involving any organ. R-CMV and end-organ disease after ASCT has not been studied thoroughly. Autograft recipients are generally considered to have low risk of R-CMV or end-organ disease.
OBJECTIVE: Evaluate the incidence, risk factors, and outcome of R-CMV in adult patients with hematologic malignancies undergoing ASCT.
DESIGN: Retrospective single center study.
SETTING: This study was approved by the institutional review board of AUBMC and conducted at our institution
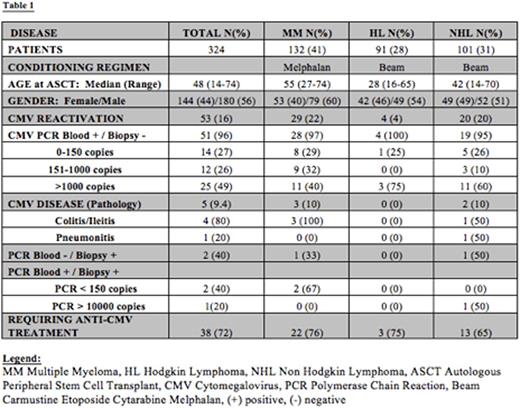
PATIENTS OR OTHER PARTICIPANTS: A total of 324 consecutive ASCT were performed at AUBMC between January 2005 and March 2016. All patients and transplant-related characteristics are listed on Table 1. CMV DNA load in blood was measured by quantitative polymerase chain reaction (PCR) weekly as a routine monitoring strategy in all patients. Irrespective of PCR results, some patients suspected to have gastrointestinal involvement were biopsied. Also, in the presence of symptomatic CMV reactivation, appropriate anti-CMV therapy was instituted.
MAIN OUTCOMES MEASURES: The primary outcome is understanding the potential relationship between R-CMV and Overall Survival (OS). Secondary outcomes included the effect of CMV reactivation on transplant related mortality (TRM), and progression free survival (PFS).
RESULTS: Overall, 53 (16%) patients had R-CMV and 38 (72%) required anti-CMV treatment. Five (1,5%) had CMV disease with positive PCR on colon biopsy, yet two had PCR negative in blood. After a median follow up of 21.5 months (range: 1 to 125 months), there was no significant difference in OS or PFS between patients with or without R-CMV. TRM has increased from 1.1% in patients with no R-CMV to 13% in patients with R-CMV (P=0.003). We didn't observe any impact for age, sex, type of disease, pre-transplant treatment types/lines on the incidence R-CMV following ASCT.
CONCLUSIONS: Our data suggest that R-CMV is not uncommon in ASCT recipients and may contribute to increased TRM. Biopsy is recommended in case of high suspicion of R-CMV irrespective of PCR results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal