Abstract
Introduction: Treatment of elderly multiple myeloma patients remains a clinical challenge. The frailty and comorbidities represent major obstacles in successful treatment. We therefore conducted a single center analysis of elderly myeloma patients in order to identify possible prognostic factors which affect their prognosis. We focused on simple clinical parameters that can be used as a clinical tool in daily practice.
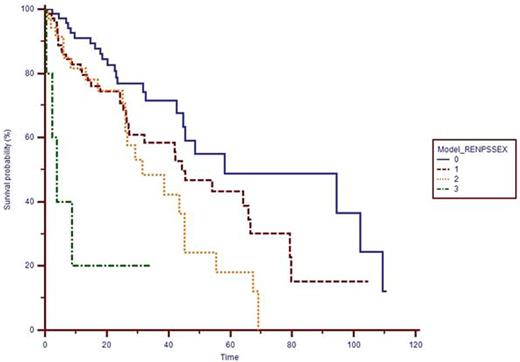
Methods: All patients treated at our department for myeloma from years 2007-2014 who were older than 65 years were included in the analysis. Demographic, baseline disease and treatment characteristics were collected. Adverse clinical characteristics were selected based on univariate analysis. These include renal insufficiency at the time of diagnosis (creatinine >2.0 mg/dL), male sex a performance status ECOG>2 on diagnosis. The simple model assigning one point for each of these factors was given to each specific patient. Overall survival was calculated based on subgroups with 0-3 points as a sole endpoint in elderly patients.
Results: We identified 184 patients (83 males and 101 females, median age 73 years) with multiple myeloma. 76 patients (41.3%) were older than 75 years, 47 (25.5%) patients had renal insufficiency, 59 (32.1%) patients were ECOG>2. Only 20 patients (10.9%) were offered autologous transplantation. 165 patients (89.7%) were treated with novel agents frontline (bortezomib, thalidomide or lenalidomide). The median overall survival was 58.2, 44.4, 31.6 and 3.9 months in groups assigned 0, 1, 2 and 3 points respectively. The differences were statistically significant (p=0.0001, log-rank test).
Conclusion: This simple model might easily identify patients at high risk of early mortality based on three simple clinical characteristics available in all patients at the time of disease onset. Model like this needs a validation using a larger cohort of patients.
Supported by PRVOUK P37.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal