Abstract
BACKGROUND: Infiltration of the spleen plays an important role in the disease progression of patients with chronic lymphocytic leukemia (CLL). Despite this fact, the role for splenectomy in the management of CLL is not well defined. Historically, splenectomy has primarily been used for management of select patients with auto-immune cytopenias (e.g. autoimmune hemolytic anemia [AIHA], immune thrombocytopenic purpura [ITP]). We conducted a retrospective study to evaluate the utility of splenectomy in CLL patients cared for at Mayo Clinic over the last 20 years.
METHODS: We used the Mayo Clinic database to identify all CLL patients who underwent splenectomy at Mayo Clinic since 1995. Medical records were reviewed to identify the indications for splenectomy, the pathologic findings at the time of surgery, and clinical outcomes. The indications for splenectomy were categorized as: diagnostic splenectomy, AIHA, ITP, symptomatic splenomegaly, and other. Pathology reports were reviewed to identify the findings at the time of surgery with respect to involvement by CLL and/or other lymphoproliferative disorders.
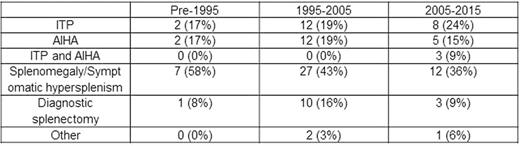
RESULTS: Of the 5333 CLL patients seen at Mayo Clinic between 1/1/1995 and 12/31/2015, 107 (2%) underwent splenectomy at Mayo. The rate of splenectomy in female subjects was 1.7% (31/1779), and the rate in male subjects was 2.1% (76/3554). Of the 2354 subjects with IGHV mutation status, the rate of splenectomy in IGHV mutated subjects was 2.1% (23/1085) compared to 0.7% (9/1269) in IGHV unmutated subjects (p=0.004). The indication for splenectomy in these 107 patients was diagnostic splenectomy in 14 (13.1%) patients, ITP in 22 (20.6%), hemolytic anemia in 19 (17.8%), ITP and hemolytic anemia in 3 (2.8%), symptomatic splenomegaly in 46 (43.0%), and 3 (2.8%) other lymphomas.
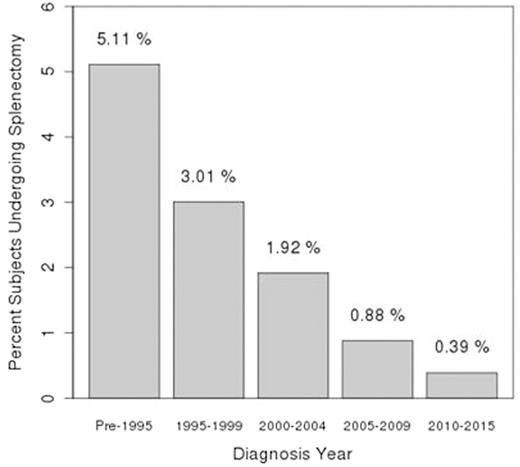
The rate of splenectomy decreased over the interval of the study (Figure). The per year risk of requiring splenectomy for patients diagnosed with CLL prior to 1995 was 0.32%/year, compared to 0.30%/year for those diagnosed from 1995-1999, 0.24%/year for those diagnosed from 2000-2004, 0.15%/year for those diagnosed from 2005-2009, and 0.16%/year for those diagnosed from 2010-2015 (p=0.01). The indication for splenectomy also changed over the study interval (Table)
Pathologic review of the spleen demonstrated normal splenic tissue in 3 (2.8%), infiltration by CLL in 99 (92.5%), involvement by diffuse large B-cell lymphoma in 2 (1.9%) and involvement by other lymphomas in 3 (2.8%; T-cell lymphoma [n=1], T-cell large granular lymphocytic leukemia [n=1], and splenic marginal zone lymphoma [n=1]).
CONCLUSION: These findings describe a large experience with the use of splenectomy in patients with CLL. Splenectomy is utilized relatively rarely (2% of CLL patients). The role of splenectomy in the management of CLL also appears to be changing with both a decreased frequency of splenectomy and a change in the indication for splenectomy over the last 2 decades. The potential benefits of splenectomy must be weighed against the know risks such as a lifelong increased risk of infection, as well as a higher risk of thromboembolism and secondary cancers.
Splenectomy Indication by Time Period of CLL Diagnosis
Parikh:Pharmacyclics: Honoraria, Research Funding. Ding:Merck: Research Funding. Shanafelt:GlaxoSmithkKine: Research Funding; Janssen: Research Funding; Genentech: Research Funding; Pharmacyclics: Research Funding; Cephalon: Research Funding; Celgene: Research Funding; Hospira: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal