Abstract
Background. The tyrosine kinase inhibitors (TKI) are the standard therapy for patients with chronic myeloid leukemia (CML) in chronic phase. However, six years after the diagnosis, only 50%-60% of CML patients are treated with the initial dosage of Imatinib, while the remained patients require a different dosage or treatment. One of the causes of resistance to TKI is additional chromosome aberrations in Ph+ cells (ACA) and BCR-ABL1 kinase domain (KD) mutations. Patients with KD mutations, (especially with mutations affecting P-loop and T315 codon) and patients with ACA in addition to the Ph-chromosome have significantly inferior unfavorable outcomes. To the best of our knowledge, the presence and the prognostic role of the two major resistance mechanisms in CML patients during TKI treatment had not been performed in combination before. The aim of our study was to evaluate the long-term impact of the simultaneous presence of BCR-ABL1 KD mutations and ACA in Ph+ cells in newly diagnosed CML patients on TKI treatment results.
Patients and methods.We analyzed charts of 30 patients with ACA in Ph+ cells, who were diagnosed with CML between 2005 and 2015. All patients received only TKI treatment. There were 14 females (47%) and 16 males (53%) with a median age of 47 years (range, 20-75). Patients' distribution for Sokal risk groups was as follows: low 6 (20%), intermediate 10 (33%), high 14 (47%) patients. Five (17%) patients had high-risk EUTOS score. Twenty-three patients had been diagnosed in the chronic phase and 7 (23%) - had the accelerated phase. Twenty-six (87%) patients started treatment with Imatinib 400 mg QD, 3 patients started with Nilotinib 400 mg BID and 1 patient started with Dasatinib 100 mg QD. The "major-route" ACA was detected in 16 (53%) CML patients. Sixteen (53%) patients had ACA at the time of initial CML diagnosis.
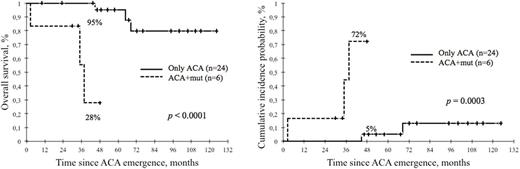
We investigated the influence of ACA and KD mutations on overall survival (OS) and CML-related death with the Cox regression method and Fine and Gray regression model. Probabilities of OS were estimated using the Kaplan-Meier method, survival times were compared with log-rank test. Cumulative incidence probability (CIP) of "death due to CML" were estimated with cumulative incidence function (causes of death unrelated to CML had to be considered as competing risks), difference between groups was assessed with Gray's test. All analyses were performed according to the intention-to-treat principle.
Results. The median follow-up from diagnosis was 77 months (range, 14-124), from ACA emergence - 51 months (3-124). Six (20%) patients died at the moment of the analysis data, 5 (17%) of them had CML progression. The combination of BCR-ABL1 KD mutations and ACA (ACA+mut) was found in 6 (20%) patients. Five different mutations (T315I, E355G, G250E, D363Y, E279K) were identified and one patient had double mutations (F359C and T315I). Forty-six percent (12/26) of Imatinib first-line treated patients were switched to second-line therapy (Dasatinib and Nilotinib), subsequently 12% (3/26) of patients were switched to Dasatinib as third-line. Among the 2nd TKI first-line treated patients: 2 (50%) were switched from Nilotinib to Dasatinib. The multivariate regression analysis had shown that the combination of BCR-ABL1 KD mutations with ACA had a prognostic significance for OS (p=0.003) and a cumulative incidence of death due to CML (p=0.0005) from the moment of ACA emergence. We also studied the influence of these factors influence on OS and CIP of death due to CML from date of diagnosis. ACA+mut co-existence (n=6) was statistically significant (p=0.02) only for CIP of death due to CML, but not for OS. On the next step, we compared the impact of combination BCR-ABL1 KD mutations with ACA on OS and CIP death due to CML following the emergence of ACA. As shown in Figure 1, patients with ACA+mut (n=6) had a lower 4-year survival rate (28%) than patients with only ACA - 95% (n=24), p<0.0001, and significantly higher CIP of death due to CML (72% vs 5%), p=0.0003. Eight-year cumulative incidence probabilities of CML-related death after diagnosis were 40% in patients with ACA and KD mutations (n=6) vs 12% in cases of only ACAs (n=24), p=0.04.
Conclusion. Our study demonstrated the significance of simultaneous presence of BCR-ABL1 KD mutations and ACA for TKI therapy outcome. CML patients with a combination of BCR-ABL1 KD mutations and ACAs conferred an inferior survival and can be viewed as the poor prognostic group.
Fominykh:Novartis Pharma: Honoraria; BMS: Honoraria. Shuvaev:Pfizer: Honoraria; BMS: Honoraria; Novartis pharma: Honoraria. Shukhov:Novartis Pharma: Honoraria; BMS: Honoraria. Chelysheva:Novartis: Consultancy, Speakers Bureau; Bristol-Myers Squibb: Speakers Bureau. Turkina:Pfizer: Honoraria; Novartis Pharma: Honoraria; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal