Abstract
Background
Chronic myeloid leukemia is a myeloproliferative neoplasm that is characterized by BCR-ABL1fusion gene and typically exhibits three distinct stages: chronic phase, accelerated phase and blast phase (BP). With tyrosine kinase inhibitors (TKIs) becoming standard front-line therapy, the progression of CML to BP has been dramatically decreased. In pre-TKI era, the blasts were of myeloid lineage in approximately 70% of patients with CML-BP, lymphoid lineage in approximately 30% of patients, and rarely, mixed phenotype. In the era of TKI era, cases of CML-BP with mixed phenotype are rarely reported to date.
Methods
Cases of CML diagnosed since year 1998 when TKI therapy was implemented in our institution to present were reviewed for blastic transformation. Clinical characteristics and laboratory data were collected. Lineage was assigned based on flow cytometry, cytochemistry or immunohistochemistry according to the 2008 WHO classification.
Results
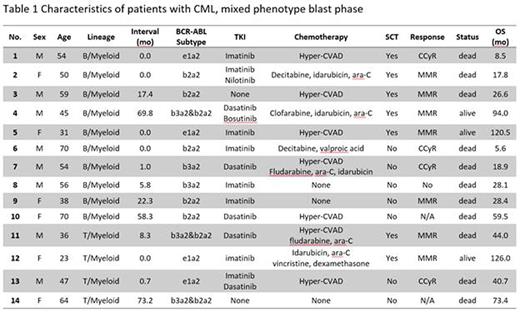
A total of 430 patients were diagnosed with CML-BP: 278 (64.7%) had myeloid BP, 138 (32.1%) lymphoid BP, and 14 (3.3%) mixed phenotype BP (Table 1). Of these 14 cases of mixed phenotype BP, 10 were of B/myeloid and 4 T/myeloid. Molecular assay showed that 4 patients had p190 subtypeBCR-ABL1transcript and the remaining 10 patients had p210 subtype. There are 8 men and 6 women. The median age at diagnosis of CML-BP was 52 (range 23-70). Five patients presented with CML-BP initially, and the remaining 9 patients developed BP later during treatment with a median interval of 17.4 months from initial diagnosis of CML to blast transformation.
Twelve of the 14 patients received TKIs, 11 patients received multi-agent chemotherapy (including hyper-CVAD regimen), and 7 patients underwent allogeneic stem cell transplantation (allo-SCT). In 12 patients with known treatment response, 11 achieved complete cytogenetic response, and 7 achieved major molecular response. Of the 7 cases treated with allo-SCT, all achieved complete cytogenetic response, and 6 achieved major molecular response. Patients with mixed phenotype BP had a slightly better prognosis than patients with myeloid or lymphoid BP. The overall survival after blastic transformation was 17.8 months (range 0.7-73.2 months) in patients with mixed phenotype BP, comparing to 9.6 month in patients with myeloid BP and 15.9 months in patients with lymphoid BP. However, limited by the small sample size, no statistical significance was reached.
Conclusion
Blastic transformation of CML with mixed phenotype is rare. The prognosis of patients with mixed BP is poor. Aggressive chemotherapy in combination with TKIs might be effective, and allo-SCT may offer a chance of deep response and probably longer overall survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal