Abstract
INTRODUCTION/ BACKGROUND
Antiphospholipid syndrome (APS) is an immunologic disorder characterized by thrombotic or obstetrical complications and persistent positivity of anticardiolipin antibodies, lupus anticoagulant, or beta-2 glycoprotein-1 antibodies. Bleeding complications in APS may sometimes occur, in the form of adrenal hemorrhage, immune thrombocytopenia (ITP), or, rarely, the lupus anticoagulant-hypoprothrombinemia syndrome (LAHS). Traditional laboratory markers of coagulation are not reliable in evaluating thrombotic or hemorrhagic risk in APS due to baseline prolongation of the prothrombin time (PT) and/or partial thromboplastin time (PTT). Thromboelastography (TEG) is a global assay of hemostasis that has been utilized in trauma surgery, emergency medicine, and chronic liver disease to identify specific coagulation defects and guide transfusion therapy. We sought to explore the role of TEG in evaluation of APS.
METHODS
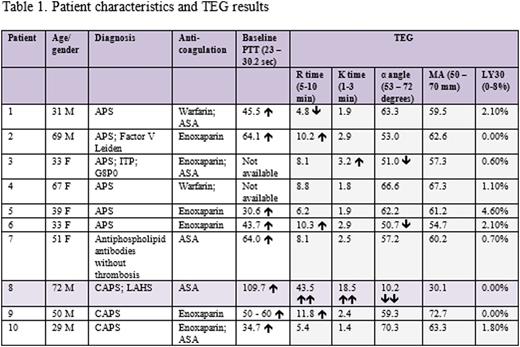
TEG was performed on whole blood obtained from 10 patients with APS (n = 6), catastrophic APS (CAPS; n = 3), or antiphospholipid antibodies without thrombosis (n = 1). Chronic aspirin (ASA) was used as monotherapy in 2 patients; 8 were on either warfarin or enoxaparin (some in combination with ASA). Immunomodulatory treatments included hydroxychloroquine, mycophenolate, azathioprine, monthly IVIG, rituximab, or eculizumab. Prior to blood collection, patients were instructed to hold ASA for 7 days, warfarin for 5 days, or enoxaparin for 2 days, as appropriate. For patients on enoxaparin in whom cessation of anticoagulation was not feasible, heparinase was added to samples for TEG measurements. The following data was compiled for each patient: baseline PTT; lupus anticoagulant, anticardiolipin IgG and IgM, and beta-2 glycoprotein-1 IgG and IgM titers; and thrombotic, hemorrhagic, and obstetrical events.
RESULTS
Baseline PTT was prolonged in most patients. TEG values were within or near the normal range in almost all cases, with no consistent differences among patients with thrombotic or obstetrical APS, CAPS, or antiphospholipid antibodies without thrombosis. R time (a measure of clot initiation) was mildly prolonged in 3 cases and minimally reduced in 1. One patient with lupus, ITP, arterial and venous thrombosis, and multiple miscarriages showed minor prolongation of K time (a measure of time to maximum clot amplification) and a slight decrease in ▢ angle (a measure of thrombin burst). LY30 (a measure of fibrinolysis) was normal in all cases. One patient with LAHS and severe hemorrhagic complications had marked prolongation of R and K times and marked reduction of ▢ angle and MA (a measure of clot tensile strength), consistent with a strong bleeding phenotype.
CONCLUSIONS
Despite abnormal baseline coagulation studies, APS patients generally do not demonstrate a major bleeding propensity in global hemostasis assays. TEG may have potential utility in identifying APS patients with bleeding due to LAHS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal