Abstract
Background: Neutropenic fever is a common complication of therapy for many cancers. Previous studies have shown high rates of in-hospital mortality ranging from 10-14% (Chindaprasirt J., et al, Asian Pac J Cancer Prev 2013; Kuderer N. M., et al, Cancer 2006; Lal A., et al,Asian Pac J Cancer Prev2008; Lyman G. H., et al,Cancer 2010). However, outcomes have not been studied in recent years since the release of updated infectious disease guidelines and improvements in supportive care.
Methods: We queried years 2009 to 2013 of the National Inpatient Sample to determine the incidence, mortality, and length of stay for neutropenic fever hospitalizations. The National Inpatient Sample is a nationally weighted sample of all hospital discharges in the United States, derived from discharge billing records from hospitals across the country. Patients aged 18 and older with a principal diagnosis of neutropenia [International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes 288.00 and 288.03] and associated fever (ICD-9-CM code 780.61) were included. Patients with multiple malignancies, no malignancies, or admitted for an obstetric procedure/complication were excluded. Baseline characteristics, associated infections, and in-hospital complications were analyzed using descriptive statistics. Mortality and length of stay were our primary outcomes. Multivariable logistic regression was performed to identify predictors of mortality and longer length of stay.
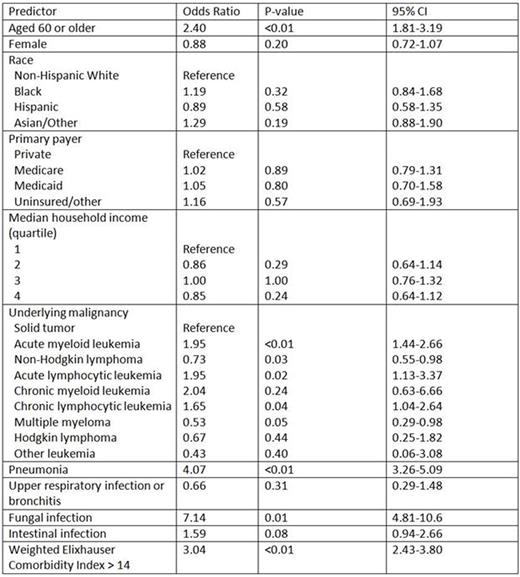
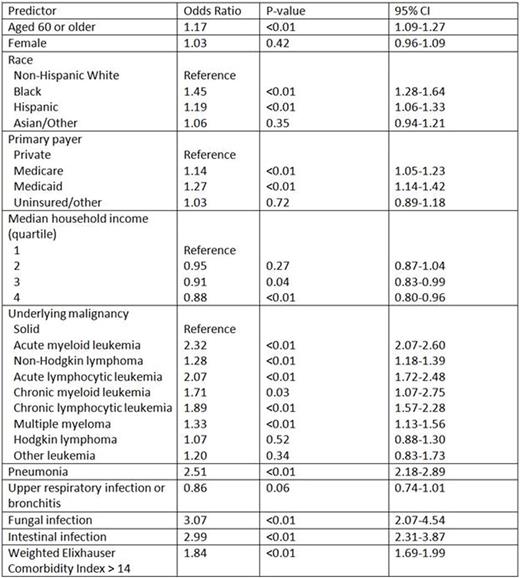
Results: A total of156,132 admissions with neutropenic fever occurred between 2009 and 2013. The average incidence of hospitalization for neutropenic fever was 85 per 100,000 total admissions, and did not change significantly over time. The distribution of admissions according to major types of malignancy was: solid tumors (54%); non-Hodgkin lymphoma (20%); acute myeloid leukemia (12%); acute lymphocytic leukemia (4%); and multiple myeloma (4%). The overall mortality was 2% and did not change significantly over time. The median length of stay was 4 days (interquartile range, 3-7). Pneumonia was the most commonly diagnosed infection (9%), followed by urinary tract infection (7%), bacteremia (4%), skin/soft tissue infection (4%), and upper respiratory tract infection/bronchitis (3%). Diagnosis of a fungal infection was uncommon (2%). Acute renal failure was the most common complication (7%), while acute respiratory failure (2%) and cardiac or pulmonary arrest (<1%) were uncommon. In multivariable analysis, age >59, acute myeloid leukemia, acute lymphocytic leukemia, and chronic lymphocytic leukemia (versus solid tumors), pneumonia, fungal infection and weighted Elixhauser comorbidity index >14 were significant predictors of mortality (Table 1) and increased length of stay (Table 2). Race, insurance, median household income, non-Hodgkin lymphoma, chronic myeloid leukemia, and multiple myeloma (versus solid tumor), and intestinal infection were also predictors of increased length of stay but not mortality.
Conclusions: Our study is the first to examine a nationally representative cohort of cancer patients in the hospital with neutropenic fever and identified a relatively low mortality rate. We identified age, underlying comorbidities, type of cancer, and type of infection as significant predictors of mortality. Given the low morbidity and mortality rate, further studies should be done to improve risk stratification of patients with neutropenic fever and prevent unnecessary hospitalization.
Predictors of in-hospital mortality in patients with neutropenic fever
Predictors of in-hospital mortality in patients with neutropenic fever
Predictors of length of stay > 2 days in patients with neutropenic fever
Predictors of length of stay > 2 days in patients with neutropenic fever
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal