Abstract
Introduction:
An estimated 30% of persons with hemophilia (PWH) in the US do not receive care at federally-funded hemophilia treatment centers (HTCs). These estimates suggest that perhaps 6,000 PWH and an unknown number of persons with other genetic bleeding disorders receive care elsewhere (non-HTC PWBD). Data on non-HTC PWBD are not collected on a regular basis nor maintained in a central database. Consequently, little is known about their characteristics, treatment, or care. CDC partnered with a national non-profit, consumer-focused organization, Hemophilia Federation of America (HFA), on the CHOICE Project to collect information on non-HTC PWBD to better estimate disease burden and inform planning, decision making, and programming. The objective of this analysis is to describe the treatment, sources, and patterns of care for non-HTC PWBD.
Methods:
From 04/2013-07/2015, HFA recruited US PWBD >/=18 years old (adults) and caregivers of children with bleeding disorders for CHOICE through email, social media, print, and word-of-mouth to take a ~20 minute survey in English or Spanish, online or on paper. Non-HTC PWBD were solicited specifically but others were not excluded from participation. Participants' status as non-HTC PWBD was determined using an algorithm based on responses to specific survey questions. For this analysis, survey elements included demographics, diagnosis, treatment regimen and treatment products used, and health services utilization (usual source of care, frequency of care, barriers to regular care, delay of care, hospital emergency room (ER) utilization, and hospitalizations within the past 12 months).
Results:
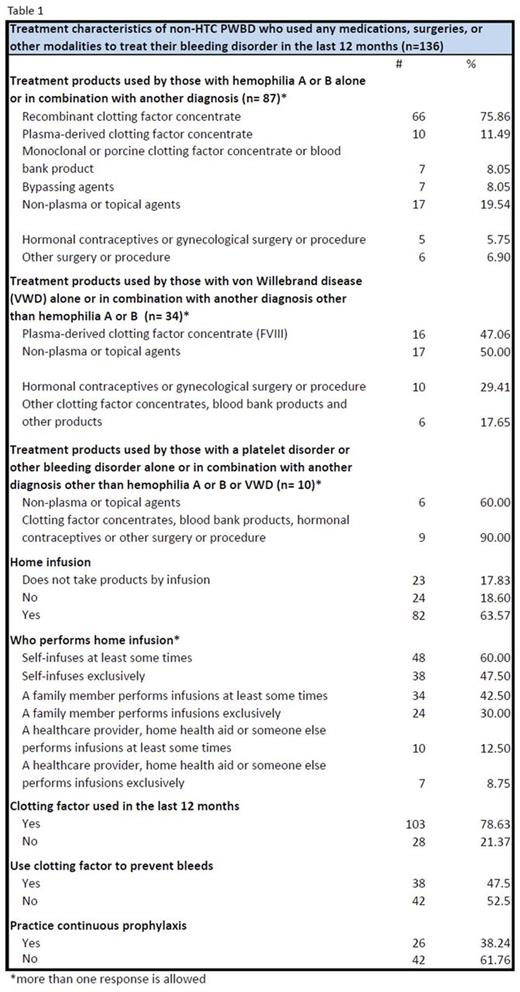
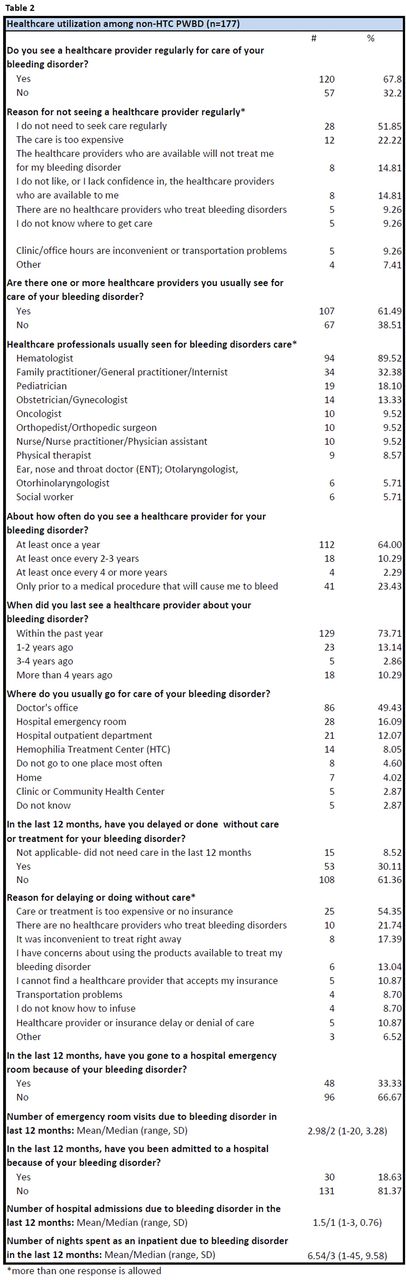
One hundred seventy-seven (22%) participants from 805 eligible surveys were identified as non-HTC PWBD: 52.5% male; 72.7% adult; mean age 33 years (±19). One hundred fifty-six (88.1%) reported a single bleeding disorder diagnosis; 21 reported multiple diagnoses. See Tables 1 and 2: The most commonly used treatments for hemophilia A or B were recombinant clotting factor concentrate (factor) (75.9%), topical or non-plasma products (e.g., desmopressin) (19.5%), and plasma-derived factor (11.5%). Non-plasma or topical products (50.0%), plasma-derived factor VIII (47.1%), and hormonal contraceptives (26.5%) were used to treat von Willebrand disease. Over 77% of those using intravenous product infused at home; 45.3% self-infused. Of those using factor, 47.5% used it to prevent bleeds with 38.2% practicing continuous prophylaxis. Approximately 32% did not visit a healthcare provider regularly for their bleeding disorder; top reasons included no need for regular care (51.9%) and expense (22.2%). One hundred seven (61.5%) respondents had one (38.1%) or more (61.9%) healthcare providers from whom they received care for their bleeding disorder. Nearly 88% (94) visited a hematologist; when a hematologist was not visited, the family practitioner was the next most common provider used (6.6%). The most common places for care were the doctor's office (49.4%), ER (16.1%), and hospital outpatient department (12.1%). In the last 12 months, 33.3% visited an ER and 18.6% were admitted to a hospital due to their bleeding disorder; 32.9% delayed or did without needed care due mostly to expense/lack of insurance (54.4%), lack of healthcare providers (21.7%), or inconvenience (17.4%).
Children were more likely than adults to: have a usual healthcare provider (75.0% vs. 56.8%, p=.03); visit a healthcare provider regularly for care of their bleeding disorder (97.9% vs. 57.0%, p<.0001); and use recombinant factor (hemophilia A or B) (96.4% vs. 66.1%, p=.002). Women delayed or did without care more than men (57.7% vs. 42.3%, p=.03).
Conclusions:
The majority of non-HTC PWBD in this project received treatment for their bleeding disorder and reported care from an appropriate health care provider; however, about 16% with needs did not see a healthcare provider regularly and over one-third delayed or did without care. This sample does not necessarily represent all non-HTC PWBD, as affiliation with an HTC was not always clear and targeted outreach by HFA Member Organizations in some regions may have led to over-representation of some participant characteristics. Additional analysis of non-HTC PWBD health outcomes is needed to determine whether those outcomes differ from other PWBD and to understand how best to identify and recruit non-HTC PWBD for surveillance.
Owens:Haplomics Inc.: Consultancy, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal