Abstract
Background: DLBCL is the most common subtype (30-40%) of non-Hodgkin lymphoma and 50-60% of patients (pts) are cured with standard R-CHOP therapy. Among pts who fail R-CHOP, only 10-20% experience prolonged disease-free intervals with high-dose chemotherapy and autologous stem cell transplant (SCT). In particular, pts relapsing within 12 months (mo) of diagnosis and/or refractory pts have a very poor outcome (Crump, ASCO 2016). In addition, many pts are SCT-ineligible due to advanced age and/or comorbidities (Friedberg, ASH Educ Program 2011). Therefore, R/R DLBCL represents a clear unmet medical need. Ibrutinib (ibr), a first-in-class, oral, once-daily inhibitor of Bruton's tyrosine kinase, has shown activity as a single agent in R/R DLBCL, particularly in the non-germinal center B-cell-like (non-GCB) subtype (Wilson, Nat Med 2015). Lenalidomide (LEN) is an immunomodulatory agent that has shown activity in combination with rituximab (RTX) in phase 2 studies of R/R DLBCL (Wang, Leukemia 2013). This multicenter, open-label, phase 1b/2 study is designed to evaluate the safety and efficacy of ibr in combination with LEN and RTX in pts with R/R DLBCL. Here, we report preliminary results of the phase 1b portion of the study.
Methods: The primary objective of the phase 1b portion is to determine the maximum tolerated dose and/or recommended phase 2 dose of ibr in combination with LEN and RTX in R/R DLBCL using a modified 3+3+3 design; the secondary objective is overall response rate (ORR) (Cheson, J Clin Oncol 2007). In phase 2, efficacy of the combination will be evaluated in R/R non-GCB DLBCL. SCT-ineligible pts, aged ≥18 years with histologically confirmed R/R DLBCL after ≥1 prior therapy, ECOG PS <2, and no central nervous system disease or history of allogeneic SCT were included. Pts received once-daily ibr (560 mg) in combination with IV RTX 375 mg/m2 on Day (D)1 of each 28-day cycle for 6 cycles and escalating doses of LEN on D1-21 of each 28-day cycle: 15 mg starting dose = Dose Level 1 (Cohort 1), 10 mg de-escalation cohort = Dose Level −1 (Cohort −1), 15 mg re-escalation cohort = Dose Level 1 (Cohort 1+), and 20 mg Dose Level 2 (Cohort 2). Dose Level Review Committee (DLRC) meetings were held for each dose level.
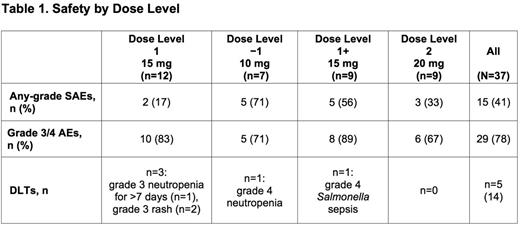
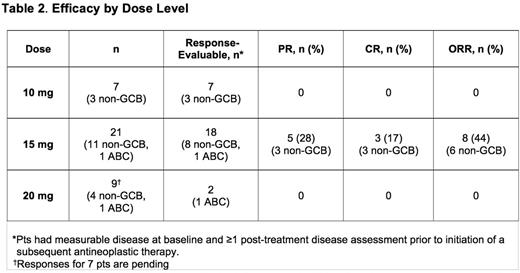
Results: Thirty-seven pts were treated across all cohorts; 20/37 had non-GCB/ABC (18 non-GCB, 2 ABC), 9/37 GCB, and 8/37 unknown DLBCL subtype;10/37 transformed disease (2 GCB, 3 non-GCB, 1 ABC, 4 unknown). Median age was 63 years (range 41-85); 16 pts (43%) were ≥65 years old. Median time from diagnosis was 14.3 mo. Pts had a median of 3 prior regimens (range, 1-5); 23 (62%) were considered refractory to their last regimen. Grade 3/4 adverse events (AEs) occurred in 29 (78%) pts. The most frequent (>10%) grade 3/4 AEs were neutropenia (32%), thrombocytopenia (14%) and maculopapular rash (11%). Any-grade serious AEs (SAEs) occurred in 15 (41%) pts (Table 1). Dose-limiting toxicities (DLTs) were observed in 5 (13%) pts (rash [2], neutropenia [2], sepsis [1]; Table 1). Due to 3 DLTs in Cohort 1, a cohort at Dose Level −1 was opened. As 1 DLT was observed at this dose level, re-escalation to higher levels (starting at 15 mg LEN) occurred. Twenty-four (65%) pts discontinued treatment due to disease progression (14/24), AE (8/24), and withdrawal of consent (2/24); 14 (38%) died, primarily due to progressive disease (n=9). Deaths due to AEs (n=4) included E. coli sepsis, cardiac arrest (after progression and subsequent antineoplastic therapy), pneumonia, and worsening DLBCL. Cause of death was unknown in 1 pt. In the response-evaluable population (Table 2), on 10 mg LEN (n=7), there were no responses. On 15 mg LEN (n=18, including 2 pts with DLTs who received ≤15 days of study drug), the ORR was 44%; there were 3 complete responses (CRs) and 5 partial responses (PRs, among them, 3 pts with refractory disease); 6/9 (67%) with non-GCB/ABC DLBCL responded (including all 3 CRs). On 20 mg LEN, 2 response-evaluable pts did not respond, other response evaluations are pending.
Conclusions: Based on safety data from the phase 1b portion of the study and the DLRC recommendation, the phase 2 portion of the study is being initiated at the 20 mg LEN dose level in combination with RTX and ibr. Preliminary efficacy results demonstrate responses at 15 mg LEN and suggest that a dose level above 10 mg LEN might be needed to induce a response in R/R DLBCL. In summary, despite small pt numbers, the results seen in this high-risk refractory DLBCL population are encouraging.
Goy:Pharmacyclics LLC, an AbbVie Company: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Genentech: Research Funding; Acerta: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; infinity: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Other: Writing support, Speakers Bureau; Johnson & Johnson: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Ghosh:Gilead: Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau; SGN: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol Myers Squibb: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding, Speakers Bureau; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pharmacyclics LLC, an AbbVie Company: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Genentech: Research Funding; TG Therapeutics: Research Funding. Dang:Eisai: Research Funding; Seattle Genetics: Research Funding; Novartis: Honoraria; Pharmacyclics LLC, an AbbVie Company: Research Funding; Valor: Research Funding; Oncomed Pharmaceuticals Inc: Research Funding. Knapp:Insys Therapeutics, Inc.: Consultancy, Other: Travel, Accommodations, Expenses; Pharmacyclics, LLC, an AbbVie Company: Consultancy, Other: Travel, Accommodations, Expenses, Research Funding. Kingsley:Pharmacyclics LLC, an AbbVie Company: Equity Ownership; Gilead: Equity Ownership. Tran:Pharmacyclics LLC, an AbbVie Company: Employment, Other: Travel, Accommodations, Expenses; AbbVie: Equity Ownership. Ping:Exelixics, Inc.: Employment, Equity Ownership; Pharmacyclics LLC, an AbbVie Company: Employment; AbbVie: Equity Ownership. Beaupre:AbbVie: Equity Ownership; Pharmacyclics LLC, an AbbVie Company: Employment, Other: Leadership; Travel, Accommodations, Expenses, Patents & Royalties, Research Funding. Neuenburg:AbbVie: Equity Ownership; Pharmacyclics, LLC, an AbbVie Company: Employment. Ruan:Celgene: Consultancy, Honoraria, Research Funding, Speakers Bureau; Pharmacyclics, LLC, an AbbVie Company: Research Funding, Speakers Bureau; Seattle Genetics: Consultancy, Research Funding, Speakers Bureau; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal