Abstract
Background: No established therapies exist for patients who fail or relapse after initial therapy for AL amyloidosis. Bendamustine has shown potential in treating multiple myeloma, chronic lymphocytic leukemia and non-Hodgkins lymphoma but it has not been well studied in AL amyloidosis. We sought to investigate the efficacy and safety of using Bendamustine in combination with dexamethasone (Ben/Dex) in patients with relapsed AL amyloidosis in a multi-center phase 2 study and present the results of the final analysis.
Methods: This Phase IIa clinical trial enrolled 31 patients who had persistent or progressive AL amyloidosis after at least 1 prior therapy. An optimal two-stage Simon design approach was used. Of 13 patients initially enrolled, 3 experienced hematologic partial response (PR), and an additional 16 were treated in the second stage. It was pre-determined that if 9 or more of the 29 patients with evaluable response had hematologic PR or better the treatment would be considered worthy of further development. Evaluable response was defined as patients who completed at least 2 treatment cycles. The primary objective was to determine the rate of partial hematologic response (PR). Secondary objectives included the overall hematologic response rate, organ response rate, toxicity profile, event free survival, and overall survival (OS). Patients received treatment in 28 day cycles with Bendamustine given on day 1 and day 2 (100 mg/m2 IV for CrCl≥60 mL/min, 90 mg/m2 IV for CrCl 59-30 mL/min, 70 mg/m2 IV for CrCl 15-30 mL/min) and dexamethasone 20-40 mg given weekly. Treatment was continued until disease progression or for up to 6 courses after complete response (CR). Reasons for discontinuation also included unacceptable toxicity, patient refusal, and non-response.
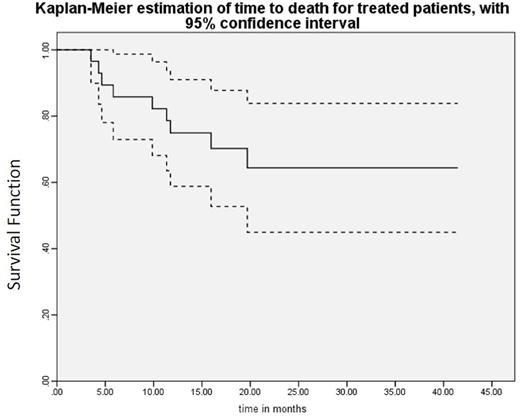
Results:Of the 31 patients enrolled in the trial, 29 had evaluable responses and completed a median of 4 cycles of therapy (range 2-12) with one patient still undergoing treatment as of 7/1/2016. Median age of enrolled patients was 64 (range 42-78). Primarily involved organs included heart (53%), kidney (36%), nerve (7%), and liver (4%); 18 patients had ≥2 major organs involved. The patients received a median of 1.5 prior treatments (range 1-4) and 13 had received prior autologous stem cell transplants. Of evaluable patients (n=29), 41% had hematologic response to Ben/Dex (3% CR, 17% very good partial response, 24% PR). Of these 13 patients, 6 had a response after only 1 cycle of therapy and the median time to best response was 1 cycle (range 1-6 cycles). The median follow up of patients was relatively long, 18.4 months (range 1.5-41.5) and the median OS has not yet been reached (Figure 1). Event free survival defined as time to death, progression of disease or initiation of new therapy was 9.24 months (range 1.8-18.0) (Figure 2). Only 3 patients discontinued treatment due to disease progression while 8 stopped due to an adverse event (AE) although 5 AEs were only grade 1-2 events. There was 1 death during treatment that was unrelated to the study drug and due to underlying cardiac amyloidosis. The most common drug related all grade AEs included anemia (9%), fatigue (8%), and nausea (7%). Organ response was observed in 5 out of 16 patients with renal involvement and 2 out of the 19 patients with cardiac involvement.
Conclusions: Bendamustine in combination with dexamethasone is active treatment in patients with AL amyloidosis who had failed multiple prior therapies and results in a significant hematologic response. Treatment was very well tolerated with a low incidence of severe AE in this delicate patient population. Therefore bendamustine is another treatment approach for AL amyloidosis patients who currently have limited therapeutic options.
Lentzsch:Foundation One: Consultancy; BMS: Consultancy; Celgene: Consultancy, Honoraria. Comenzo:Karyopharm: Research Funding; Prothena: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; Takeda: Consultancy, Research Funding. Zonder:Celgene: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Prothena: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Bristol Myers Squibb: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Pharmacyclics: Other: DSMC membership. Pregja:Takeda: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Research Funding; Seattle Genetics: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Prothena: Consultancy, Honoraria; Bristol Myers Squibb: Consultancy, Honoraria; Pharmacyclics: Other: data safety monitoring committee. Landau:Prothena: Honoraria, Membership on an entity's Board of Directors or advisory committees; Spectrum Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees; Onyx/Amgen: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal