Abstract
Introduction
In AML patients (pts) undergoing 7+3 induction chemotherapy (IC), incomplete platelet (plt) recovery can lead to increased risks of bleeding, prolonged dependence on plt transfusions, plt alloimmunization, and can hinder post-remission therapy. Eltrombopag is a thrombopoietin receptor agonist that stimulates megakaryopoiesis and has anti-leukemic effects (Erickson-Miller 2008; Will 2009; Roth 2012). We present results of an interim, prespecified analysis of an ongoing trial [ClinicalTrials.gov Identifier: NCT02071901] evaluating the efficacy of eltrombopag in accelerating plt count recovery in older AML pts (>60 years) receiving IC.
Methods
All newly diagnosed AML pts >60 years (yrs) with ECOG scores of 0-2, no active second malignancy, and no evidence of marrow fibrosis at the time of AML diagnosis were included. Acute promyelocytic leukemia, acute megakaryocytic leukemia, and AML out of myeloproliferative neoplasms were excluded. IC consisted of an anthracycline (daunorubicin at 45_mg/m2 or idarubicin at 12 mg/m2 x 3 days) and infusional cytarabine (100 mg/m2 x 7 days). Eltrombopag was administered starting day 15 (range, day 15-18) of IC in pts who had no morphological evidence of disease (marrow blasts <5%) on day 14 (range, day 14-17). The primary endpoint was the proportion of pts achieving plt>50000/µL by day 24 of IC. Eltrombopag was administered at a dose of 200 mg (100 mg for East Asian [EA] pts) daily with a one-time maximal dose escalation to 300 mg daily (150 mg in EA pts) if plt remained<50,000/µL after 2 weeks on treatment. Eltrombopag was discontinued once plt exceeded 100,000/µL. A two-stage accrual design with a maximum accrual goal of 31 eligible pts was employed with early stopping if>5 of 12 initial eligible pts (42%) failed to achieve plt>50,000/ µL by day 24. Informed consent was obtained prior to start of IC.
Results
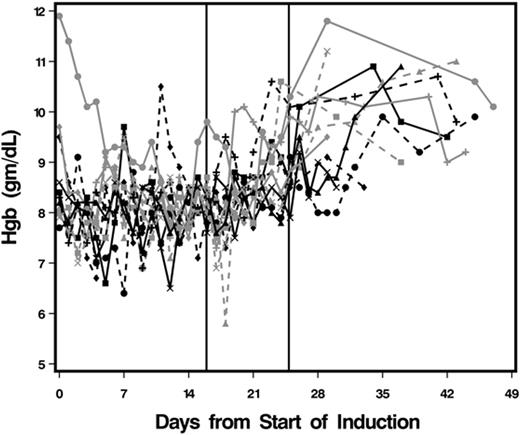
Between 9-2014 and 6-2016, 34 pts were consented of whom 13 met the eligibility criteria. Reasons for failing eligibility (21/34 pts, 62%) included >5% blasts on day 14 marrow (n=15); acute clinical worsening (n=3); marrow fibrosis at AML diagnosis (n=1); active second malignancy (n=1); and elevated transaminases (n=1). Characteristics of the study cohort were: 54% females, 1 pt of EA heritage, median age of 64 yrs (range, 60-71), and 75% with good ECOG status (ECOG 0 or 1). Most pts (62%) had de novo AML, 38% had secondary AML (therapy-related or prior MDS). By CALGB criteria, 82% had intermediate cytogenetics, 9% had adverse karyotype and in 9% cytogenetic analysis was unsuccessful. The median eltrombopag treatment duration was 10 d (range, 8-14 d), and no dose escalations were required. Pts received a median of 4 units of plt (range, 3-11), which equated to 1 unit every 3.6 d, during induction, while during the eltrombopag treatment period, the median requirement decreased to 2 units (range, 0-6) or 1 unit every 4.8 d (p=.04). Pts were transfused with a median of 7 units of red blood cell (RBC) (range, 3-17; 1 unit every 2d) during induction, while on eltrombopag, the median RBC unit transfusion requirement decreased to 4 (range,1-7; 1 unit every 3.6 d) (p=.02). 92% of pts achieved CR at a median time of 32.5 d from IC (range, 29-42). One pt had incomplete CR due to poor ANC recovery. Median times from the start date of IC to plt>20,000/µL,>50,000/µL, and>100,000/µL were 19 d (range, 15-24), 24 d (range, 21-33), and 25 d (range, 23-33), respectively. By day 24 of IC, 8 of 13 pts (62%) had plt>50,000/µL. Trends in the levels of hemoglobin, absolute neutrophil count (ANC), and plt count over time along with median eltrombopag start and stop times are shown in Figure 1. The median peak plt count reached on eltrombopag was 719,000/µL (range, 280-1,935,000/µL). The median time to reach peak plt count from start date of eltrombopag was 19 d (13-28 d). The reported toxicities were all grade 1/2 and included nausea (n=2), decreased vision (n=1), elevated transaminases (n=1 each), and one each with hypokalemia and hypomagnesaemia.
Conclusions
Our interim analysis suggests that eltrombopag can hasten plt recovery, potentially reduce plt transfusions and increase CR rates in older AML pts undergoing IC without any limiting toxicities.The initial cohort does not show evidence for acceleration of the leukemic process and progression stopping milestones were not reached. The study met its interim objectives and is currently accruing pts.
Mukherjee:Celgene: Consultancy, Honoraria, Research Funding; Ariad: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal