Abstract
Background: Ibrutinib, an inhibitor of Bruton's tyrosine kinase, is indicated for the treatment of several B-cell malignancies. In the phase 3 HELIOS trial, the addition of ibrutinib to a bendamustine plus rituximab regimen significantly improved patient outcomes, including quality of life, overall response, and progression-free survival, in patients with relapsed/refractory chronic lymphocytic leukemia (CLL; Chanan-Khan, Lancet Oncol 2016; 17:200-211). Here we report the results from analyses exploring the pharmacokinetic (PK) interactions between ibrutinib, bendamustine, and rituximab from the HELIOS trial.
Methods: In total, 578 patients were randomized to 420 mg ibrutinib (n = 289) or placebo (n = 289) in combination with 6 cycles of bendamustine and rituximab until disease progression or unacceptable toxicity. The bendamustine intravenous (IV) dose was 70 mg/m2 on days 2-3 of cycle 1 and days 1-2 of cycles 2-6; the rituximab IV dose was 375 mg/m2 on day 1 of cycle 1 and 500 mg/m2 in cycles 2-6. Infusion durations were typically 30 min for bendamustine and varied based on tolerability and infusion rates for rituximab.
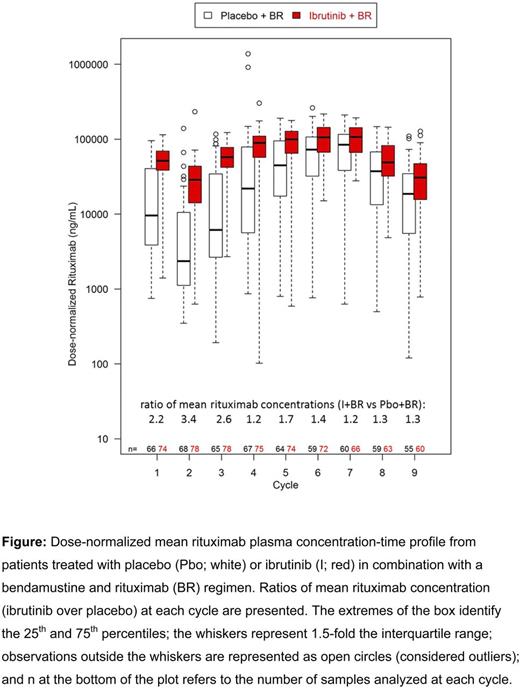
Ibrutinib PK samples were collected from all patients at predose, 1, 2, and 4 hr on day 1 of cycles 1 and 2. In a subset of patients, bendamustine PK samples were collected on day 2 of cycles 1 and 2 at predose, end of infusion, and at 1, 2, and 4 hr. Rituximab PK samples were collected on days 1 (predose) and 15 of cycle 1, day 1 (predose) of cycles 2-6, and on day 1 of cycles 7-9. Dose-normalized bendamustine and rituximab concentration-time data were stratified by treatment to evaluate the effect of ibrutinib on the PK of these drugs. Descriptive statistics were calculated using R (www.R-project.org).
Results:PK samples from 178 patients were analyzed; 84 patients from the placebo arm and 94 patients from the ibrutinib arm. The mean dose ± standard deviation (SD) of bendamustine was 68.2 ± 6.3 mg/m2 and 68.9 ± 4.7 mg/m2 in patients receiving ibrutinib and placebo, respectively; the doses of rituximab were 468.1 ± 55.3 mg/m2 and 465.2 ± 65.0 mg/m2, respectively. The dose-normalized plasma concentration-time data of bendamustine (a cytochrome P450 1A2 substrate) from both arms were comparable, indicating that ibrutinib did not alter bendamustine PK. In contrast, systemic exposure of rituximab was higher in patients coadministered with ibrutinib than in patients who received placebo; mean predose serum concentrations were 2- to 3-fold higher in the first three cycles and 1.2- to 1.7-fold higher in subsequent cycles (Figure).
The systemic exposure of ibrutinib (n = 280; mean area under the plasma drug concentration-time curve at steady state ± SD = 447.5 ± 298.2 ng•h/mL) in patients receiving the 420 mg dose was comparable to exposures observed in studies of single agent ibrutinib (Marostica, Cancer Chemother Pharmacol 2015; 75:111-121), indicating that bendamustine and rituximab did not impact the PK of ibrutinib.
No relevant differences in safety profile were observed between the ibrutinib and placebo arm with the increase in systemic exposure of rituximab. All-grade infusion-related reactions were more frequent with placebo than with ibrutinib (22% vs. 16.7%, respectively), and the incidence of chills was comparable (~11%). Dose interruptions, dose reductions, and discontinuations due to infusion-related reaction were more frequent in the placebo arm (34.8% vs. 27.9%). Additional analyses to model the rituximab PK data using metrics of tumor burden as covariates (e.g., sum of the products of diameters) are currently ongoing and will be presented.
Conclusions:Coadministration of ibrutinib with bendamustine and rituximab did not affect the PK of bendamustine or ibrutinib but led to greater dose-normalized systemic exposure of rituximab when compared to patients who received placebo. Rituximab has been reported to be characterized by target-mediated drug disposition (TMDD; Li, J Clin Pharmacol 2012; 52:1918-1926), which may describe many rituximab PK features, such as PK differences in CLL, non-Hodgkin's lymphoma, and rheumatoid arthritis and the dependency of PK behavior on baseline tumor burden. TMDD may account for the rituximab PK findings from this study, with the early decreased tumor burden following ibrutinib resulting in decreased rituximab clearance and hence higher systemic exposure. The clinical significance of this finding needs additional exploration.
Cramer:Mundipharma: Other: Travel, Accommodations, Expenses; Janssen-Cilag: Consultancy, Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Astellas: Other: Travel, Accommodations, Expenses; Novartis: Consultancy, Research Funding; GlaxoSmithKline: Research Funding; Roche: Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Gilead: Other: Travel, Accommodations, Expenses, Research Funding. Demirkan:Amgen: Consultancy. Fraser:Celgene: Research Funding; Janssen: Honoraria, Research Funding, Speakers Bureau. Bartlett:Pharmacyclics: Research Funding; Janssen: Research Funding. Dilhuydy:Gilead: Honoraria; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Honoraria. Loscertales:Roche: Honoraria, Speakers Bureau; Gilead Sciences: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Goy:Genentech: Research Funding; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pharmacyclics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Infinity: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Writing support, Speakers Bureau; Acerta: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau. Ganguly:Seattle Genetics: Speakers Bureau; Janssen: Research Funding; Onyx: Speakers Bureau. Poggesi:Janssen: Employment, Equity Ownership. de Jong:Janssen: Employment. Neyens:Janssen: Employment. Salman:Janssen Research & Development: Employment, Equity Ownership, Other: Travel, Accommodations, Expenses. Howes:Janssen Research & Development: Employment. Mahler:Janssen Research & Development: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal