Abstract
BACKGROUND The evaluation of response to therapy in CLL is widely assessed according to the iwCLL guidelines which define progressive disease (PD) as advancing lymphocytosis, lymphadenopathy, organomegaly, cytopenias or histological transformation (Hallek, Blood, 2008). At the time of PD, considerable heterogeneity exists; patients (pts) with asymptomatic lymphocytosis seem to have a more indolent clinical course than those who progress by other means. On this basis, we hypothesized that the type of PD might impact on subsequent post-progression pt outcomes including the time to next treatment (TTNT) and overall survival (OS).
METHODS All analyses were performed on data collected from pts enrolled in the CLL11 trial (NCT01010061), an open-label, randomized, pivotal phase III study comparing the efficacy and safety of obinutuzumab (GA101; GAZYVA) plus chlorambucil (Clb) with rituximab and Clb or Clb alone in treatment-naïve pts with CLL and pre-existing comorbidities (Goede, NEJM, 2014).
Pts with defined PD, excluding death, were identified and assigned to 1 of 2 groups according to whether PD was by absolute lymphocyte count (ALC), or other, (non-ALC) causes, as per iwCLL criteria. Individuals could be allocated to only 1 group. To test whether subgroups were balanced at baseline (BL), characteristics between groups were compared for proportional differences using a Pearson chi-square test.
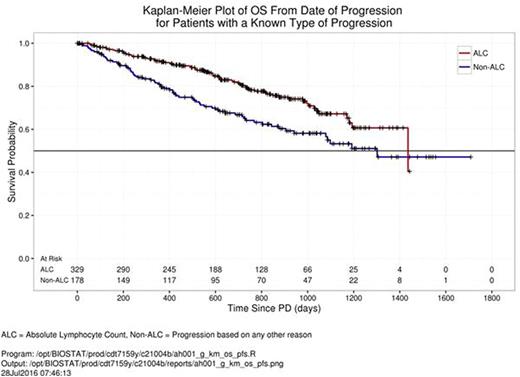
Post-progression Kaplan-Meier survival curves for TTNT and OS were plotted by PD type. The log-rank test was used to detect significant differences in the treatment timings and survival distributions between groups, respectively.
Group differences in the proportion of pts with cytopenia due to bone marrow (BM) infiltration (excluding autoimmune causes) were tested at BL and the time of PD. Similarly, B symptoms were calculated as the proportion of pts reporting disease-attributable fevers, night sweats or weight loss.
Health-related quality of life (HRQoL) data were extracted from the EORTC QLQ-C30 and -CLL16 questionnaires. The mean and mean change scores by progression type were derived from BL and PD assessments.
RESULTSOf the 781 pts enrolled in CLL11, progression data were available for 507 (64.9%) subjects. Of these, a total of 329 (64.9%) pts progressed by ALC, while the remaining 178 (35.1%) had PD from an alternative, non-ALC cause. At study BL, there were no differences in the demographics or disease characteristics between groups.
The median post-progression TTNT for the ALC group was 373 days (95% CI [320, 449]) versus 120 days (95% CI [101, 209]) for the non-ALC group, (p < 0.0001) (Fig 1). Type of PD was also associated with a better OS in the ALC group (p = 0.0014) but the median time could not be accurately estimated due to insufficient events (Fig 2). A higher proportion of non-ALC pts demonstrated evidence of disease-related BM infiltration at PD (0.38 vs 0.24, p = 0.0013) with anemia (0.24 vs 0.10, p < 0.001) and neutropenia (0.16 vs 0.06, p < 0.001) representing the greatest differences between groups (Fig 3). Despite a trend towards a higher proportion of B symptoms in the non-ALC group at PD, significance was not achieved (p = 0.0624).
Mean absolute HRQoL scores at BL, highlighted trends towards a higher level of functioning (higher scores) and milder physical symptoms (lower scores) in the ALC group. At the time of PD, those progressing by ALC reported clinically meaningful (6 point) higher role and physical functioning and measurably less fatigue, insomnia, dyspnea and pain.
Within-group, mean score changes between BL and PD highlighted an overall trend towards improved functioning (QLQ-C30) over the course of treatment in the ALC group and a decline in function in the non-ALC group although differences were small. In general, both groups reported milder disease-related symptoms (QLQ-C30 and -CLL16) at PD with pts in the ALC group showing clinically meaningful improvements in fatigue and appetite.
CONCLUSION These data provide the first comprehensive outcome analysis in CLL based on the mode of first progression for pts receiving upfront chemoimmunotherapy. We have shown that progression by ALC is consistently associated with a favourable clinical profile but whether our findings apply to pts in the relapsed setting or to those receiving other novel therapies is yet to be determined. An accurate estimate of survival by PD type might guide physician choice/timing of next treatments.
Bazeos:Roche: Employment. Gower:Roche Products Ltd: Employment. Swann:Roche: Employment. Trask:Genentech, Inc.: Employment, Equity Ownership. Dixon:Roche Products Limited: Employment, Equity Ownership. Crompton:Roche: Employment. Kinnersley:Roche-Genentech: Employment, Equity Ownership. Al-Sawaf:Gilead: Other: Travel grants. Goede:Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees; GlaxoSmithKline: Honoraria; Roche: Consultancy, Honoraria, Other: Travel grant, Research Funding. Fingerle-Rowson:F. Hoffmann-La Roche Ltd: Employment, Equity Ownership. Humphrey:Genentech, Inc.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal