Abstract
Background: The EUMDS registry, collecting prospective observational data on lower-risk MDS (LR-MDS) patients from 142 centers in 17 countries, is performing a study on the hypothesized negative impact of red blood cell transfusions (RBCT) on outcome in LR-MDS. The aim of this study istoevaluate in transfusion dependent (TD) patients temporal changes in iron metabolism and presence of potentially toxic forms of iron, measured as labile plasma iron (LPI) and their impact on oxidative stress, using malondialdehyde (MDA), and their impact on survival.
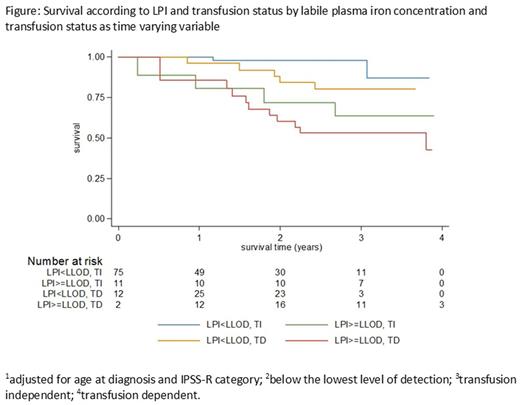
Methods: We analyzed serum samples from 100 LR-MDS patients at 6-month intervals fortransferrin saturation (TSAT), non-transferrin bound iron (NTBI) and LPI.Cox proportional hazards regression models and Kaplan-Meier (KM) survival curves were used in time-to-event analyses to assess the impact of LPI, NTBI and TSAT by transfusion status. All variables were treated as time-varying covariates in the model by assessing the levels of the parameters: LPI, NTBI (<LLOD vs elevated), TSAT (<80% vs ≥80%) and transfusion status (TD vs transfusion independent (TI)) at each visit.We also explored in 56 patients the temporal prevalence of oxidative stress and its relation with toxic iron species by means of the MDA assay in paired samples with at least 1-year interval.
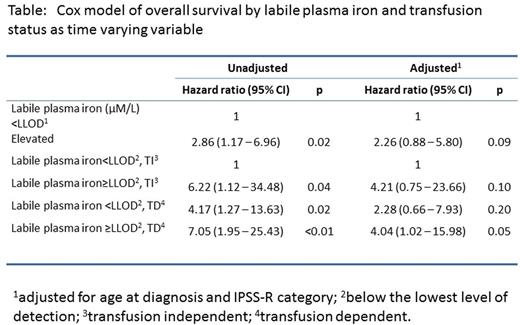
Results: Themedian age was 73 years.IPSS-R risk groups of this cohort of LR-MDS, defined as IPSS low & intermediate-1 risk, were: very low 32%, low 41%, intermediate 8%, high 3% and unknown 16%. Patients were subdivided in ring sideroblastic MDS (RS-MDS) (34%) and non-RS-MDS (64%). Both groups were subdivided in TD and TI patients.Elevated LPI in combination with high TSAT (>80%) occurred almost exclusively in patients with TI RS-MDS and in all TD MDS patients.Time-dependent, multivariate analysis (MVA), adjusting for age and IPSS-R risk group, of elevated LPIconcentrations for overall survival (OS) resulted in a Hazard Ratio (HR) of 2.3 with 95%CI (0.9-5.8). Elevated NTBI was associated with HR of 0.7 and 95%CI: 0.3-1.8 and TSAT >80% with HR of 0.9 and 95%CI: 0.3-2.6.MVA of OS by LPI and transfusion status as time varying variable showed a significant impact of elevated LPI in the TD group only(HR=4.0, 95%CI: 1.02-15.9) (p = 0.05).
MDA concentrations were measured in 28 patients with RS-MDS and 28 non-RS-MDS patients. 21 and 29 patients were TD at time of 1st and 2nd MDA measurement respectively. The overall median MDA concentrations in the 1st sample were elevated compared to controls: 0.9 (0.3 - 4.1) (range controls: 0.16 to 0.64 mM) and remained elevated in the 2nd sample. Median MDA increased from 0.8 to 0.9 mM in the MDS-RS group (p = 0.008 paired one-sided T-test). Significantly higher MDA concentrations were observed in TD patients at time of the 2nd measurement: a median MDA level of 0.7 mM (0.3 - 3.6) in TI and 1.3 (0.3 - 6.8) in TD patients resp. (p = 0.01). MDA levels did not increase in time in TI MDS, but showed a trend to higher MDA in 9 patients who became TD between 2 MDA measurements (p=0.11) and in the 21 patients TD before the 1st measurement (p = 0.12). Median MDA did not change in time in the majority of patients with LPI levels below the detection line (<LLOD). The correlation between elevated LPI and MDA concentrations was weak (r = 0.047, P = 0.82). Paired analysis of the 16 patients with LPI < LLOD at time of 1st measurement and elevated LPI at time of 2ndmeasurement showed a slight increase (p = 0.10) of the median MDA levels from 1.1 to 1.2mM/l. The impact on OS of lowest 50% of MDA levels at each measurement and the highest 50% of MDA levels, adjusted for MDS-RS status, TD and LPI>LLOD vs <LLOD was not evident with an unadjusted HR of 1.3 (0.6 - 3.1) and an adjusted HR of 0.6 (0.2 - 1.5).
Interpretation:Iron toxicity and increased oxidative stress occurred in all types of TD MDS patients and in TI RS-MDS patients. This study illustrates LPIas a clinically relevant assay for identification of the toxic fraction of iron overload and its negative impact on overall survival. In contrast, high TSAT (>80%) and elevated NTBI concentrations did not predict survival.Oxidative stress, using MDA as a measurement of lipid peroxidation, is increased in the majority of lower-risk MDS patients, usually early after diagnosis. The highest MDA levels are measured in patients receiving RBCT, but the LPI and MDA were not correlated, which can be explained by the slower clearance of MDA after RBCT compared to the more rapid clearance of LPI.
Symeonidis:Takeda: Consultancy, Honoraria; Amgen: Honoraria; Roche: Honoraria; Genesis: Honoraria. Smith:Jansen Cilag: Research Funding; Novartis: Research Funding; Amgen: Research Funding; Celgene: Research Funding. de Witte:Incyte: Consultancy; Celgene: Consultancy; Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal