Abstract

INTRODUCTION
MDS are a heterogeneous group, and it is necessary an adequate prognostic stratification in order to the best management. The new revised international prognostic scoring system (IPSS-R) has improved prognostic ability for survival and AML evolution comparing with the previous prognostic indexes. But, it is not clear the prognosis of patients included in the intermediate group, 20% of MDS, patients with a median OS of 3 years according to Greenberg et al, are they in the high or in the low risk category? The aims of the present study were to describe characteristics of patients included in this intermediate group of the IPSS-R in the Spanish MDS cohort and to identify which factors could have an impact on survival. A new score prognostic system (GESMDi score) in order to a better stratification should be proposed in this subset of patients that will be useful for determine the best therapeutic approach for them.
METHODS: All patients were included in the GESMD, diagnosed of Primary MSD and Intermediate IPSS-R. The Statistical analyzes were performed using SPSS version 21, Cox models and Kaplan-Meier curves were used to demonstrate clinical outcomes. Regarding the new score proposed, GESMDi score, modeling of prognostic risk was based on multivariate analysis of survival time. Cox model for survival was built to derive the relative weights within the score.
RESULTS: Data from 957 patients of 69 centers of GESMD were evaluated. Their median age was 73.9 years (p25/p75 66-80), 61.6% males (N=590), and median follow-up 21,4 months (p25-p75 de 11-41). Regarding WHO 2001 classification: 31% were RAEB-1, 21% CMML, 18% RCMD, 14% RAEB-2, 3% RCMD-RS, 3.1% RARS, 2.5% RA, 2% 5q-syndrome, 2% AML, 1% unclassified. Median hemoglobin at diagnosis was 9.8 g/dL (p25/p75:8.3-11.6), median bone marrow (BM) blasts 6% (p25/p75:3-8) and median platelet count 99x109/L (p25/p75:66-180). According to IPSS, 5% of patients were classified as low risk, 78% as intermediate-1, 16% as intermediate-2 and 1% as high risk. Cytogenetic were very good in 2% of patients, good in 76%, intermediate in 17%, poor in 5% and in 1% very poor. IPSS-R score classified patients in 3 different groups, with a punctuation of≤ 3.5 (35.6%), >3.5 and ≤ 4 (35.8%) and> 4 and ≤ 4.5 (28.5%).
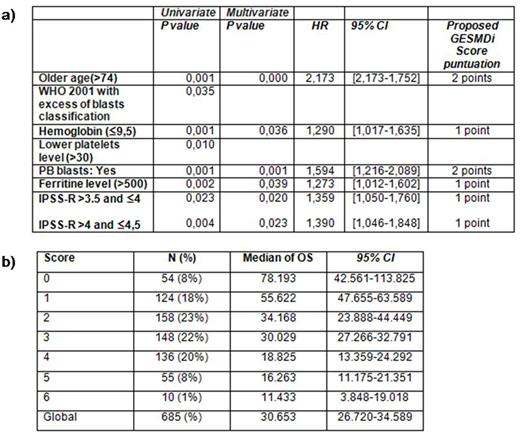
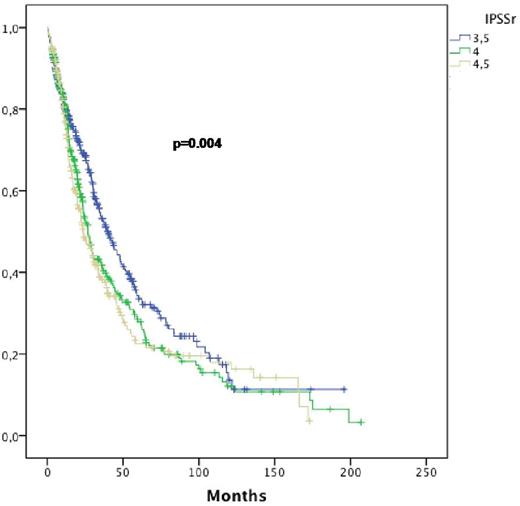
Median OS was 30.1 months, the estimated 1-year and 2-y OS were 79.2% and 57.8%, respectively. In the univariate analysis for OS older age (>74y, p<0.001), lower Hb level (≤9.5 g/dL, p<0.001), WHO 2001 with excess of blasts classification (p=0.035), lower platelets level (≤30 x 109/L, p=0.01), PB blasts (yes, p=0.001), ferritine level (>500 ng/ml, p=0.002), and higher IPSS-R score (>3.5 and ≤ 4 and >4 and ≤ 4.5, p=0.023 and p=0.004, figure 1) had a deleterious impact on survival. In the multivariate analysis, only age, Hb level, PB blast, ferritine level and IPSS-R value retained statistical significant impact on OS (table 1a). In the multivariate analysis, Hazard ratio, a new score system (GESMDi score) was established for all patients. Patients with adverse features were added points in order to stratify the risk of death: age<74y and/or PB blasts (2 points) and Hb level ≤9.5 g/dL and/or ferritine level >500 ng/ml and/or IPSS-R of >3.5 (1 point), table 1a.
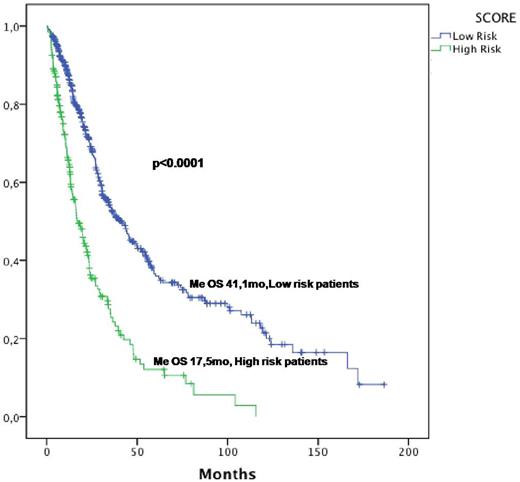
The GESMDi score was performed in 685 patients with all data available and 7 groups of patients were defined with different median OS (p<0.0001, table 1b). Two final categories were established according to the definition of risk from the Spanish MDS group, low risk patients (estimated OS >30 months) and high risk patients (<30 months). Patients with scores between 0-3 (70.6% patients, me OS 41.1, 95CI 34.4-47.7) were in the low risk definition while patients with scores between 4-6 (29.3% patients, me OS 17.5 mo, 95CI 13.4-21.5) were classified as high risk patients (p< 0.0001, Figure 2).
CONCLUSIONS: GESMDi score, a proposed prognostic score system from patients with intermediate IPSS-R, allow us to establish a better prognosis stratification in this heterogeneous MDS population. Treatment and management should be better established for those patients nowadays according to this novel stratification.
a) Univariate and multivariate analysis for OS among patients with Intermediate IPSS-R b) OS according to the GESMDi score proposed
a) Univariate and multivariate analysis for OS among patients with Intermediate IPSS-R b) OS according to the GESMDi score proposed
OS according to IPSS-R value in the intermediate group (≤3.5, ≤4 and ≤4.5)
OS according the GESMDi score proposed in the intermediate IPSS-R group: low and high risk patients (n=685)
OS according the GESMDi score proposed in the intermediate IPSS-R group: low and high risk patients (n=685)
Del Cañizo:Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Astex: Membership on an entity's Board of Directors or advisory committees; janssen: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Díez Campelo:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Astex: Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding; celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal