Abstract
Introduction:
BRCA1 plays a key role in maintaining genomic stability and interacts directly with several proteins that regulate hematopoietic stem cell functions and are part of the Fanconi anemia (FA) double-strand break (DSB) repair pathway. Loss of BRCA1 in murine bone marrow causes hematopoietic defects similar to those seen in FA (Vasanthakumar, Blood 2016). BRCA1 is highly expressed in hematopoietic tissues, whereas its expression is lost in CML (Deutsch et al, Blood 2003) and t-AML (Scardocci et al, Br J Cancer 2006). Since FA is associated with an increased risk of developing myelodysplastic syndromes (MDS), we examined the protein expression of BRCA1 and three other important components of the FA DNA repair pathway, as well as PARP-1, whose co-alteration with BRCA causes synthetic lethality.
Methods:
We recently established a tissue microarray (TMA) with bone marrow biopsies from 119 MDS patients, 40 AML patients, and 11 normal controls. Biopsy material was retrieved from the Institute of Pathology, Heinrich-Heine-University Düsseldorf, Germany. The TMA was produced at SciLifeLab Tissue Profiling Facility in Uppsala, Sweden. Immunohistochemistry (IHC) protocols were established in our lab for the detection of BRCA1, BRCA2, FANCD2, H2AX, and PARP1. Semi-quantitative analysis was done according to Remmele-Stegner immunoreactive score (IRS) with a point system from 0 to 12. Expression was categorized as absent (0-2), weak (3-4), moderate (5-8) or strong (9-12). For correlating protein expression with clinical data from the Düsseldorf MDS Registry, samples were dichotomized into 'low expression' (1-4) and 'higher expression' (5-12). Prognostic analysis was restricted to 80 MDS patients who did not receive disease-modifying therapy.
Results:
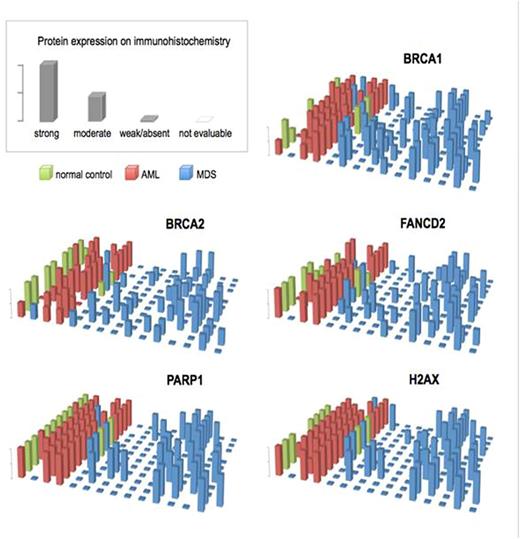
Similar to normal controls, most patients with AML showed strong expression of the proteins under consideration (Fig. 1). In contrast, low expression was found in about 60% of MDS patients. Most MDS patients showed concordant, dichotomous expression of all five proteins (either all up or all down). Correspondingly, the protein expression landscapes look similar (Fig. 1). Almost perfect concordance was noted for PARP1 and H2AX.
Low expression of FA/BRCA pathway proteins was not correlated with MDS type (WHO 2008) or IPSS-R risk group. Patients with higher expression of at least 3 of the 5 proteins survived longer (45 vs. 26 months) and had a longer time to AML development (median not reached at 180 months vs. 53 months), but the differences did not reach statistical significance (p=0.108 and p=0.159, respectively). Interestingly, patients with low expression of PARP1 were significantly more likely to show any chromosomal aberration (p=0.02) or an unfavourable karyotype (intermediate, high-risk or very high risk according to IPSS-R) (p=0.016). The same was true for patients with low expression of H2AX (p=0.013 and p=0.01).
Conclusions:
This is the first TMA-based investigation of FA/BRCA pathway protein expression in MDS. In stark contrast to AML, 60% of MDS patients showed low protein expression in a concordant manner. This could reflect synexpression of genes that share common cis- and trans-acting control elements. Alternatively, it could be the result of aberrant splicing, since at least 50% of MDS patients have spliceosome mutations that render a large spectrum of messenger RNAs susceptible to nonsense-mediated decay. Abnormal splicing factors may also influence the stability (and thus expression) of certain proteins through abnormal protein-protein interactions. Further IHC analyses will show whether the dichotomous protein synexpression pattern we observed in MDS extends to proteins that are unrelated to DNA maintenance.
Underexpression of FA/BRCA pathway proteins may cause chromosomal instability, as suggested by our finding of significantly more frequent karyotype anomalies in patients with low PARP1 or H2AX expression. This is in accordance with the known role of H2AX as suppressor of oncogenic chromosome translocations, and with an accelerating effect of PARP1 deficiency on centrosome amplification in BRCA1-deficient cells. FA/BRCA pathway protein underexpression may not only contribute to a better understanding of MDS versus AML pathogenesis, but may also have therapeutic implications, e.g. by affecting the response to treatment with hypomethylating agents, which are known to promote DNA double strand breaks.
Gattermann:Celgene: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Other: travel, accomodation expenses, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal