Abstract
Introduction. Myelofibrosis is a disease characterized by aberrant bone marrow function with eventual fibrosis. Current widely-used disease prognostic indices, such as the Dynamic International Prognostic Scoring System (DIPSS) do not take into account comorbidities, which may have significant effects on patient survival as well as disease course. We sought to describe the comorbidity distribution in this patient population and assess the impact of comorbidities as scored by two different widely used scales in clinical practice, the Adult Comorbidity Evaluation 27 (ACE-27) and the Hematopoietic Cell Transplant Comorbidity Index (HCT-CI), on overall survival and leukemic transformation in myelofibrosis. A score of 3 on ACE-27 or ≥3 on HCT-CI generally indicates a high burden (severe) comorbidities.
Methods. We conducted a retrospective study of 309 patients seen at the MPN program at the Princess Margaret Cancer Centre, with a confirmed diagnosis of myelofibrosis [primary myelofibrosis (PMF), post-essential thrombocytopenia (PET-MF) or post-polycythemia vera (PPV-MF)]. Patients were seen from 1999-2014 with a median follow-up time of 2 years. Time to death and leukemic transformation was examined from the date of first presentation to our centre. Our primary aim was to examine the impact of comorbidity scores, as assessed by ACE-27 and the HCT-CI, on overall survival. In a secondary analysis we examined the impact of comorbidity scores on leukemic transformation. Multivariable Cox proportional hazards models were constructed for the primary and secondary outcomes. A series of descriptive analyses were carried out examining the distribution of various comorbidities as captured by the two scales.
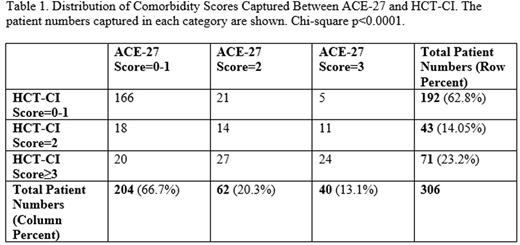
Results. The most common comorbidities captured by ACE-27 were hypertension (n=92, 22.3%), diabetes mellitus (n=43, 10.4%), venous disease (n=26, 6.3%), solid tumour including melanoma (n=26, 6.3%), and angina/coronary artery disease (n=23, 5.6%). The most common comorbidities captured by HCT-CI were cardiac (n=49, 17.3%), diabetes (n=43, 15.2%), mild hepatic (n=28, 9.9%), cerebrovascular disease (n=25, 8.8%), prior solid tumour (n=24, 8.5%). The distribution of comorbidity scores as compared between scales is shown in Table 1.
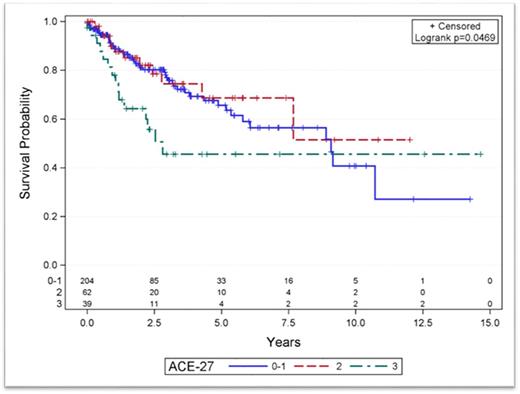
A total of 78 patients (25.2%) experienced the primary outcome of interest, which was all-cause death. For the primary outcome of overall survival, there were differences across groups of patients with different comorbidity scores using ACE-27 or HCT-CI, with the highest severity groups having worse outcomes (Figure 1). Progressively increasing DIPSS categories (Low, Intermediate-1, Intermediate-2, and High risk) were also associated with worse overall survival. On multivariable survival analysis, an ACE-27 score of 3 when compared to a lower score of 0-1 was associated with an almost two-fold increase in the risk of all-cause death [HR 1.95 (95% CI 1.06-3.58), p=0.03]. On multivariable analysis, an HCT-CI score of 3+ when compared with 0-1 was marginally significantly associated with an increased risk of all-cause death [HR 1.60 (95% CI 0.96-2.68), p=0.07]. Interaction terms were tested between the scores and age at presentation and no effect of age on survival across varying severities of comorbidities was found. In our secondary analysis, there was no impact of the ACE-27 or HCT-CI on leukemic transformation.
Conclusions. ACE-27 picked up severe co-morbidities in 13% of patients in our cohort while HCT-CI picked up severe comorbidities in 23%. Although the incidence of severe co-morbidities was lower when assessed by ACE-27, the overall impact on survival of severe comorbidities as assessed by both scores is likely to be similar. The presence of severe comorbidities at the time of diagnosis conferred a significant survival disadvantage in patients with myelofibrosis, but had no impact on progression to leukemic transformation.
Overall survival by ACE-27 comorbidity category, showing differences between categories of comorbidity severity (p=0.047, log rank test).
Overall survival by ACE-27 comorbidity category, showing differences between categories of comorbidity severity (p=0.047, log rank test).
Panzarella:Cellgene: Consultancy. Schimmer:Novartis: Honoraria. Schuh:Amgen: Membership on an entity's Board of Directors or advisory committees. Yee:Novartis Canada: Membership on an entity's Board of Directors or advisory committees, Research Funding. Gupta:Novartis: Consultancy, Honoraria, Research Funding; Incyte: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal